In a significant breakthrough in the battle against esophageal squamous cell carcinoma (ESCC), researchers have developed an enhanced prognosis prediction model that leverages detailed lymph node assessment following neoadjuvant chemoradiotherapy (NCRT). This new model promises to revolutionize the way clinicians evaluate patient outcomes and tailor treatment strategies, addressing a critical gap in effective prognosis prediction for a cancer type known for its aggressive nature and poor survival rates.
The study, encompassing 282 ESCC patients treated with NCRT followed by surgical intervention, focused on extracting nuanced lymph node characteristics that extend beyond traditional staging. Conventional pathology N (pN) staging primarily considers the presence and number of positive lymph nodes but often fails to capture deeper biological and anatomical complexities influencing patient prognosis. By evaluating factors such as the total number of lymph nodes removed, their size, anatomical location, intra-nodal tumor regression grade (LN-TRG), and extracapsular invasion, the researchers have constructed a model that surpasses standard staging in predictive accuracy.
One of the key findings highlighted is the relationship between the extent of lymph node clearance during surgery and overall survival (OS). Intriguingly, patients who had between 17 and 30 lymph nodes removed exhibited significantly better OS compared to those with fewer than 17 or more than 30 nodes cleared. This suggests an optimal surgical clearance threshold that balances maximal disease eradication without unnecessary tissue removal, potentially preserving immune function and reducing surgical morbidity.
Furthermore, the assessment of tumor regression within lymph nodes (LN-TRG) emerged as a potent prognostic factor. Lower LN-TRG, indicative of better tumor response to neoadjuvant therapy within lymph nodes, correlated strongly with improved OS and recurrence-free survival (RFS). This insight underscores the importance of not only the presence of metastatic disease but also the dynamic tumor response within the nodal microenvironment post-treatment.
Extracapsular invasion of lymph nodes, a pathological finding denoting tumor extension beyond the nodal capsule, was associated with poorer OS and RFS. This feature likely represents a more aggressive disease phenotype with enhanced potential for systemic dissemination, thus marking it as a vital element within the prognostic model.
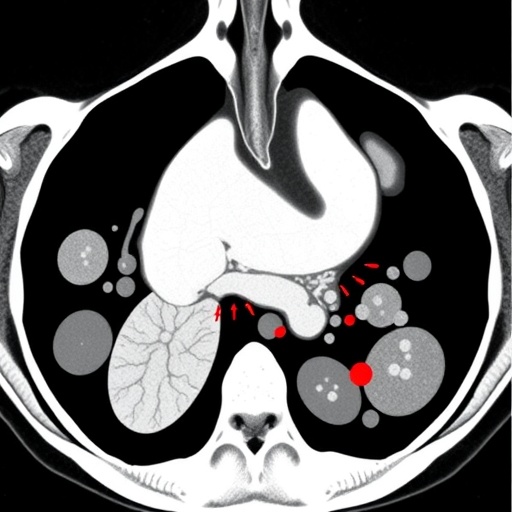
Anatomical lymph node location also played a critical role in prognosis prediction. Abdominal lymph nodes, in particular, were identified as harboring the highest ratio of residual cancer cells after therapy. These nodes demonstrated the greatest hazard ratio for adverse outcomes and contained the largest number and proportion of positive cases, highlighting their significance in guiding post-surgical management and surveillance strategies.
To distill the complex array of lymph node variables into a clinically applicable tool, the research employed advanced statistical approaches including Lasso regression and Cox univariate analysis. These methods identified five paramount factors for prognosis: LN-TRG, total tumor diameter within lymph nodes, clearing 17–30 lymph nodes, proportion of positive lymph nodes, and presence of extracapsular invasion. Integrating these variables into a comprehensive predictive model produced impressive risk stratification capabilities for both OS and RFS, with area under the curve (AUC) values of 0.705 and 0.679 respectively, outperforming pN staging.
This multifaceted model promises to improve clinical decision-making by providing a more precise prognosis, enabling oncologists to identify high-risk patients who might benefit from intensified adjuvant therapies or closer surveillance. Moreover, it offers a personalized approach to lymph node evaluation post-neoadjuvant therapy, acknowledging the heterogeneity of treatment response and disease biology within the lymphatic system.
The study’s revelations carry profound implications for the surgical management of ESCC. Recognizing an optimal lymph node clearance range challenges the prevailing surgical dogma and may influence future guidelines to strike a balance between thorough disease removal and preservation of host defenses. Additionally, the prognostic weight of extracapsular invasion and tumor regression within nodes advocates for meticulous pathological examination and standardized reporting protocols.
From a research perspective, these findings pave the way for future explorations into the molecular underpinnings of nodal tumor regression and extracapsular spread. Understanding the biological mechanisms driving these phenomena could unlock novel therapeutic targets aimed at enhancing neoadjuvant therapy efficacy and curbing metastatic potential.
The predictive model also serves as a prototype for integrating multifactorial lymph node assessments in other cancers treated with neoadjuvant modalities. By illustrating the additive value of parameters like tumor regression grade and extracapsular invasion, the study sets a precedent for refining prognostication in complex oncologic landscapes where conventional staging falls short.
Clinicians and researchers alike stand to benefit from the enhanced prognostic accuracy of this model, translating into improved patient stratification and potentially better survival outcomes. As esophageal cancer continues to pose significant treatment challenges worldwide, advancements such as these offer a beacon of hope, bringing personalized medicine to the forefront of clinical oncology.
In sum, the development of a comprehensive lymph node evaluation system post-neoadjuvant therapy represents a paradigm shift in esophageal cancer prognosis, advocating for more sophisticated pathological assessments and data integration to inform clinical strategies. This approach underscores the evolving nature of cancer care, where precision and individualized treatment outlook are paramount.
The remarkable strides made in this study underscore the necessity of revisiting and refining existing cancer staging systems. Such innovation is critical in addressing the complexity of tumor biology and treatment response, ultimately aiming to enhance patient survival and quality of life.
As this enhanced prognosis prediction model gains traction, its incorporation into routine clinical workflows could become a standard of care, guiding therapeutic decisions and optimizing resource allocation in oncology settings worldwide.
This research not only enriches our understanding of lymph node dynamics in ESCC but also exemplifies the transformative potential of detailed pathological evaluation coupled with advanced statistical modeling in shaping the future of cancer prognosis.
The potential clinical utility of this model extends beyond survival prediction, potentially informing surgical approaches, postoperative surveillance, and the selection of candidates for adjuvant therapies, thereby personalizing patient management in a truly holistic manner.
Ongoing validation and prospective studies will be essential to confirm the model’s applicability across diverse populations and clinical scenarios, ensuring its robustness and generalizability in everyday oncology practice.
Overall, this innovative lymph node assessment framework signifies a vital advance in esophageal cancer research, carrying the promise of enhanced prognostic precision and improved patient outcomes through tailored therapeutic strategies.
Subject of Research: Prognosis prediction in esophageal squamous cell carcinoma (ESCC) through advanced lymph node evaluation after neoadjuvant chemoradiotherapy.
Article Title: Enhanced prognosis prediction model in esophageal cancer via lymph node assessment post-neoadjuvant.
Article References:
Zhou, Y., Xiao, M., Li, J. et al. Enhanced prognosis prediction model in esophageal cancer via lymph node assessment post-neoadjuvant. BMC Cancer 25, 1468 (2025). https://doi.org/10.1186/s12885-025-14785-7
Image Credits: Scienmag.com
DOI: https://doi.org/10.1186/s12885-025-14785-7