Credit: Copyright UCLouvain
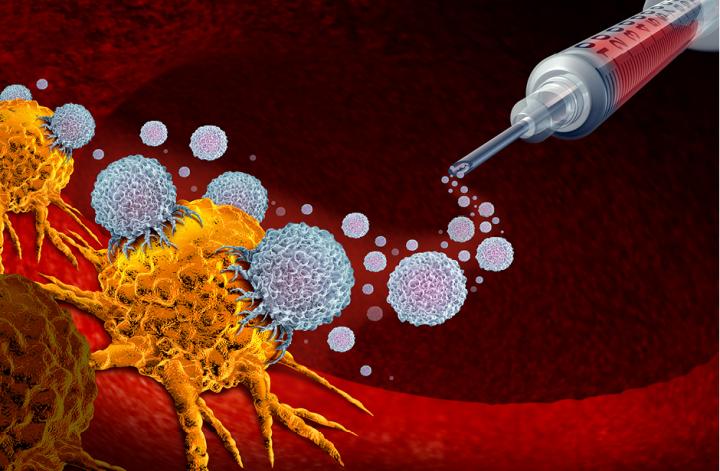
Sophie Lucas, a researcher at the University of Louvain (UCLouvain) de Duve Institute, studies the immune responses that cancer patients can develop against their own tumour. ‘In the long run,’ Prof. Lucas says, ‘the goal is to try to manipulate immune responses to make them more effective and enable the patient to reject tumour cells.’ This would be an incredible breakthrough in the field of immunotherapy, which is itself an ideal alternative to cancer therapies that target tumour cells, such as chemotherapy or radiation therapy. Immunotherapy targets immune system cells in order to stimulate them to turn against the patient’s tumour and destroy it.
Prof. Lucas’s major breakthrough? Developing a new drug that is now being tested in cancer patients for targeting their immune system. To achieve this result, the UCLouvain team made major discoveries over the past ten years. The first step: ‘In 2004, we wondered whether certain cells of the immune system could play a negative role in cancer patients’, Prof. Lucas explains. The team looked at regulatory T cells (Tregs), which can be very toxic to cancer patients: they regulate the immune system so much that they decrease the efficiency of immune cells (which are supposed to kill cancer cells). As a result, the immune system ceases to be effective at fighting cancer’s advance.
The second step: Prof. Lucas’s team learned how Tregs managed to decrease the effectiveness of anti-tumour immune cells, through the production of an inter-cellular messenger (TGF-beta) which transmits information from Tregs to other cells. This messenger has the ability to inhibit anti-tumour immune cells, thereby reducing their effectiveness. In 2009, the team realised that Tregs needed another molecule to produce these messengers: a sort of accomplice, called GARP. Thus, in just a few years, Prof. Lucas’s team identified Tregs, TGF-beta and GARP as three major players that decrease anti-tumour immune responses.
Next, the UCLouvain team observed that the administration of an anti-GARP monoclonal antibody could cure cancer in mice. ‘The results aren’t published yet’, Prof. Lucas says. ‘However, it seems that the drug works in mice. It induces the rejection of certain tumours.’ This promising discovery attracted a pharmaceutical company’s interest. ‘Human clinical trials have just started. A few cancer patients have been injected with our anti-GARP monoclonal antibodies.’
What’s next?
If clinical trials yield encouraging results, the team will have access to biopsies taken from patients treated with the anti-GARP antibody. ‘That’ll be the moment to confirm whether it works and try to foresee combining it with other anti-tumour drugs to improve effectiveness.’ The team will continue to work on the fundamental aspects of TGF-beta and GARP biology. ‘We know cells other than Tregs produce these “messengers”, but we don’t know why.’ Is it to systematically decrease immune responses? Or do they play other roles? ‘To better understand the biology of these amazing molecules, we’ll expand our area of expertise, which is currently focused primarily on cancer, to chronic infections or autoimmune diseases, for example’. When could an effective drug appear? ‘It’ll take another three to five years to see whether our drug shows signs of efficacy without excessive toxicity for cancer patients.’
Every two years the Belgian Academy of Medicine GSK Award recognises work in vaccinology and immunology that contributes significantly to basic or clinical knowledge and might impact patients. This year Sophie Lucas and her team won for their decade of research on tumour immunology.
###
Media Contact
Isabelle Decoster
[email protected]
32-486-426-220
Original Source
https:/




