In a groundbreaking step forward in ovarian cancer research, scientists have unveiled a comprehensive classification tool that deciphers the evolving immune landscape of ovarian tumors between initial diagnosis and relapse. This study, spearheaded by Denarda Dangaj Laniti and Eleonora Ghisoni at Ludwig Lausanne, represents the largest comparative analysis to date of immune profiles in both primary and recurrent ovarian cancers, offering fresh perspectives that could revolutionize therapeutic approaches for a malignancy notorious for its poor prognosis after recurrence.
Ovarian cancer remains the deadliest gynecological malignancy worldwide, partly due to its high rates of relapse and resistance to conventional therapies. While prior knowledge underscored the role of the immune system in modulating patient outcomes, there was a profound gap in understanding how the immune microenvironment transforms as the cancer returns. This research directly addresses that knowledge deficit by systematically categorizing tumors based on their immune cell infiltration, thereby revealing critical associations between immune phenotypes, genomic features, and therapeutic response.
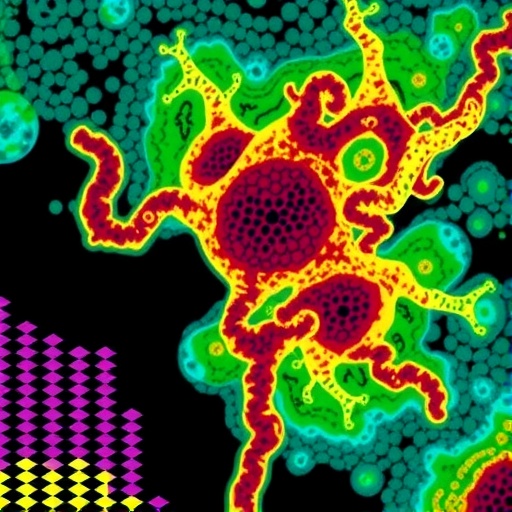
Central to this study is the novel immune classification system developed by the Ludwig Lausanne team, which analyzed nearly 700 tumor samples from five separate clinical cohorts. Utilizing digital pathology and immunohistochemical techniques focused on the presence of CD8+ T lymphocytes—key effectors in anti-tumor immunity—the researchers delineated four distinct immunologic subtypes of ovarian tumors. Tumors densely infiltrated by T cells were labeled as “purely inflamed,” whereas those with moderate infiltration earned the “mixed-inflamed” marker. Tumors exhibiting T cells only at their edges were designated “excluded,” and those lacking appreciable T cells altogether were termed “desert” tumors.
.adsslot_dPC26WxXDn{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_dPC26WxXDn{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_dPC26WxXDn{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
These immunologic designations proved to be robust predictors of patient survival outcomes. Patients harboring either purely inflamed or mixed-inflamed tumors exhibited significantly prolonged survival compared to those with excluded or desert phenotypes. Importantly, the study uncovered a strong link between tumors harboring mutations in DNA repair genes—most notably BRCA1 mutations—and the inflamed immune microenvironment. Such genetic defects appear to foster enhanced immunogenicity, thereby coupling DNA repair deficiency with favorable chemotherapy responses and extended patient survival.
But the immune complexity of ovarian tumors extends beyond T lymphocyte populations. Myeloid cells, including macrophages and dendritic cells, also occupy pivotal niches within the tumor microenvironment and influence immune dynamics. Macrophages can polarize toward states that either support anti-tumor immunity or suppress it, while dendritic cells orchestrate the activation and priming of T cells. The researchers demonstrated that upon relapse, tumors proficient in DNA repair tend to recruit immunosuppressive macrophages characterized by the expression of lipid metabolism-related proteins ApoE and Trem2. These macrophages contribute to an environment hostile to effective immune clearance and correlate with more resistant tumor phenotypes.
A key translational discovery from this research is the therapeutic potential of targeting Trem2-positive macrophages. Using mouse models, the team showed that employing an antibody inhibitor against Trem2 boosted chemotherapy response and delayed tumor recurrence, suggesting a promising new avenue for patients with tumors that fall into the immunologically “desert” category.
Conversely, tumors classified as purely inflamed and deficient in DNA repair maintain complex networks of TILs and dendritic cells that foster sustained anti-tumor immunity. These immune niches, resilient even after disease recurrence, are further supported by the recruitment of macrophages with anti-tumor functionality, highlighting the interdependence of different immune cell types in maintaining tumor control.
However, even these seemingly immune-favorable tumors are not impervious to immune evasion mechanisms. The study revealed that cancer cells in inflamed, DNA repair-deficient tumors activate a COX enzyme-driven molecular pathway upon treatment with chemotherapy and the PARP inhibitor olaparib—a drug clinically employed for BRCA-mutated ovarian cancer. This pathway elevates the secretion of prostaglandin E2 (PGE2), a lipid mediator that impairs the survival and functionality of tumor-infiltrating lymphocytes by inducing their functional exhaustion and apoptosis.
Importantly, the research team demonstrated that supplementing standard chemotherapy and olaparib with COX inhibitors in murine models significantly extended survival by counteracting PGE2-mediated immunosuppression. When combined further with checkpoint blockade immunotherapy—agents designed to reinvigorate exhausted T cells—the survival benefit was amplified, effectively doubling survival time in these preclinical models.
These findings point to a future in which ovarian cancer treatment is tailored not only on the basis of tumor genetics but also by the precise immune composition of the tumor microenvironment. Patients with inflamed, DNA repair-deficient tumors emerge as ideal candidates for combination immunotherapy trials, while those whose tumors exhibit immunosuppressive myeloid infiltration may gain clinical benefit from emerging therapies that inhibit immune checkpoints and myeloid regulators such as Trem2.
The study underscores a paradigm shift toward integrated therapeutic strategies that simultaneously target malignant cells and the immune components enabling immune evasion. By illuminating the interplay between tumor genomics and the immune microenvironment across the course of disease progression, the findings chart a course toward improved personalization of ovarian cancer therapy, with the potential to significantly alter patient outcomes.
This research was supported by the Myeloid Cells in Cancer Initiative of the Ludwig Institute for Cancer Research, the U.S. Department of Defense, and Hoffmann-La Roche AG, emphasizing the collaborative and multidisciplinary effort required to tackle the complexities of cancer immunology.
Subject of Research: Immune classification and therapeutic targeting of ovarian cancer relapse
Article Title: Immunologic evolution of ovarian tumors defines therapeutic vulnerabilities at relapse
News Publication Date: July 31, 2025
Web References:
– https://www.cell.com/cancer-cell/fulltext/S1535-6108(25)00276-4
– https://www.ludwigcancerresearch.org/ludwig-link/december-2024/a-ludwig-lausanne-collaboration-takes-aim-at-myeloid-cells-in-cancer/
– https://www.ludwigcancerresearch.org/news-releases/ludwig-cancer-research-study-identifies-cellular-interactions-essential-to-the-immune-attack-on-ovarian-tumors/
– https://www.ludwigcancerresearch.org/news-releases/immune-networks-in-tumors-prime-responses-to-a-personalized-immunotherapy/
Image Credits: Ludwig Cancer Research
Keywords: ovarian cancer, tumor microenvironment, immunology, immunotherapy, cancer relapse, DNA repair deficiency, T lymphocytes, macrophages, Trem2, COX pathway, PGE2, checkpoint blockade
Tags: CD8+ T lymphocytes in cancer therapycomparative analysis of immune profilesdigital pathology in cancer researchgenomic features of ovarian tumorsimmune cell infiltration in tumorsimmune classification system for tumorsimmune landscape of ovarian tumorsimmunohistochemical techniques in oncologyimproving prognosis in ovarian cancerovarian cancer relapsetherapeutic approaches for ovarian cancerunderstanding the immune microenvironment