In this collection of studies published in the Journal of Pediatric Rehabilitation Medicine experts document the shifts in age and ethnicity of spina bifida patients and highlight the emerging trends in caring for these patients
Credit: Developmental Pediatrics at Texas Children’s Hospital, Baylor College of Medicine, Houston, TX.
Amsterdam, NL, January 15, 2020 -In this collection of articles in the Journal of Pediatric Rehabilitation Medicine (JPRM) experts highlight the emerging trends in spina bifida care in response to challenges faced by spina bifida patients and their physicians due to demographic shifts in age and ethnicity and other societal factors.
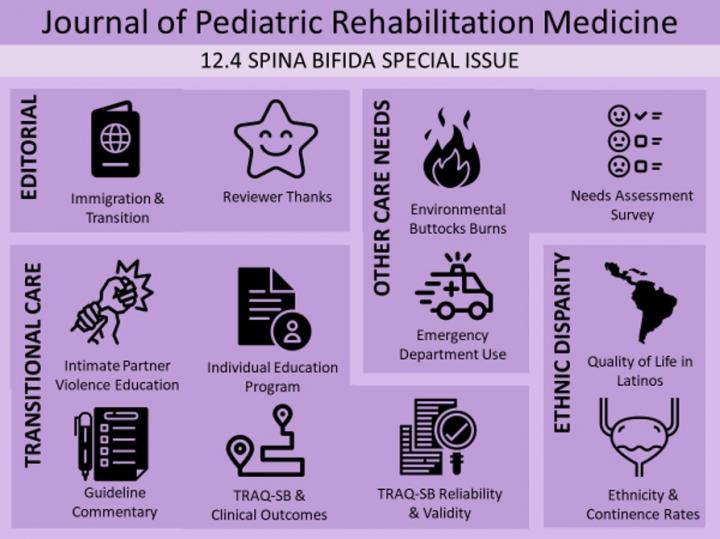
Focusing on health disparities, transitional care, and other care needs, this special issue is guest-edited by Timothy J. Brei, MD, Department of Pediatrics, Division of Developmental Medicine, Seattle Children’s Hospital, and University of Washington School of Medicine, Seattle, WA, and Jonathan Porter Castillo, MD, MPH, Director of the Spina Bifida Program within the Meyer Center for Developmental Pediatrics at Texas Children’s Hospital, Baylor College of Medicine, Houston, TX.
Spina bifida is a birth defect that occurs when the spine and spinal cord fail to form properly. Depending on the type of defect, its size, location, and complications, it can range from mild to severe and can also differ between individuals. Investigators have begun to recognize existing disparities within growing minority populations affected by spina bifida. Neural tube defects like anencephaly and spina bifida have a birth prevalence of nearly six per 10,000 live births in the US. Prevalence rates of spina bifida are also influenced by the mother’s race/ethnicity; Hispanics/Latinos consistently have a higher birth prevalence of spina bifida compared with the other racial and ethnic groups in the US.
The number of immigrants, refugees and internally displaced persons around the globe is escalating. At the same time these individuals are also living longer, so these demographic shifts in age and ethnicity are giving rise to a new era in care for patients with spina bifida. “While immigration is often a result of social determinants, including political discrimination, poverty, education, and work-related prospects, immigration itself can also be conceptualized as a social determinant of health,” explained Dr. Castillo.
Dr. Brei noted, “A call has gone out for multicenter learning collaboratives to face these newfound challenges. An example of such emergent learning collaboratives is the American Academy of Pediatrics (AAP) Spina Bifida Transition Project sponsored by the Centers for Disease Control and Prevention (CDC), an approach in accordance with the recently published Guidelines for the Care of People with Spina Bifida.”
In the US, 25% of children live in immigrant families, and of the estimated 55 million Latinos, nearly three of every four speak Spanish at home. Even so, there is a lack of research on quality of life (QOL) and social determinants of health among patients living with spina bifida. At the same time, in spite of Congress’s NIH Revitalization Act of 1993, calling for efforts to ensure that minority groups are included in representative numbers in research studies; few health-related QOL studies have documented inclusion of Spanish-speaking Latinos.
A study conducted at Baylor College of Medicine undertook a systematic review of the scientific literature on language and Latino immigrants in the US living with spina bifida. Eighteen studies met the inclusion criteria (children and adolescents 5-21 years of age with spina bifida and/or myelomeningocele; quantitative studies; health-related QOL outcome measured by validated instrument determinants; and US-based studies). Researchers concluded that QOL in individuals with spina bifida is mediated by a wide range of interrelated factors. They recommend that, in order to better serve this vulnerable population as they transition across the lifespan, multilingual condition-specific QOL measures need to be developed further and implemented among Latino individuals with spina bifida, especially those who are recent immigrants.
“The Spina Bifida Association has updated the spina bifida healthcare guidelines. Therefore, nationally and internationally, we now have guidance and the opportunity to care for all individuals as whole persons as they transition across the continuum of care, holistically approaching them in their language and cultural context,” stated Dr. Castillo. “Globally, there has been a 49% increase in immigration since 2000, thus linguistically-congruous study of QOL has increasing relevance not only locally, but also abroad.”
“In the face of the documented demographic shifts and demonstrable health disparities, the need for timely and culturally competent studies among Hispanics/Latinos, who have the highest spina bifida prevalence, is self-evident,” commented Dr Brei and Dr Castillo.
A study conducted at the University of Pittsburgh School of Nursing evaluated the feasibility of implementing a brief educational training program based on an evidence-based intimate partner violence (IPV) intervention in a pediatric spina bifida clinic. Frequency of IPV discussion was assessed through patient feedback evaluation and provider surveys.
“The educational intervention increased provider comfort with addressing IPV within a specialty clinical setting,” commented lead investigator Brenda Cassidy, DNP, University of Pittsburgh School of Nursing, University of Pittsburgh, Pittsburgh, PA. “The frequency of IPV communication by spina bifida patients significantly increased, both immediately and at two months, compared to baseline. Patients reported the discussions were beneficial, and providers reported greater comfort discussing IPV and referring patients to resources.”
The issue covers also the following topics: differences in continence rates based on ethnicity; environmental buttocks burns in children and adolescents; emergency department utilization among pediatric spina bifida patients; needs assessment survey for children and adults; an assessment of the degree to which of adolescents and emerging adults with spina bifida understand their individual education programs; two studies on use of a Transition Readiness Assessment Questionnaire (TRAQ-SB); and guidelines for the transition of young spina bifida patients to adult healthcare.
“The commentaries and original research published in JPRM will continue to serve as a catalyst for culturally-competent research, as well as thoughtful investigation and comparative analysis of management practices in order to improve the care among the diverse and aging community of individuals affected with spina bifida around the world,” concluded Dr Brei and Dr Castillo.
“Improving the health of children and adolescents with complex medical needs by disseminating peer-reviewed research worldwide is a core mission of JPRM. I am grateful for the dedication of Dr. Brei and Dr. Castillo and all the researchers and contributors to the journal. This special spina bifida issue brings together a wonderful collaboration of international experts,” added Elaine Pico, MD, Editor-in-Chief, JPRM, Pediatric Rehabilitation, UCSF Benioff Children’s Hospital Oakland, CA.
###
Media Contact
Diana Murray
[email protected]
718-640-5678
Related Journal Article
http://dx.




