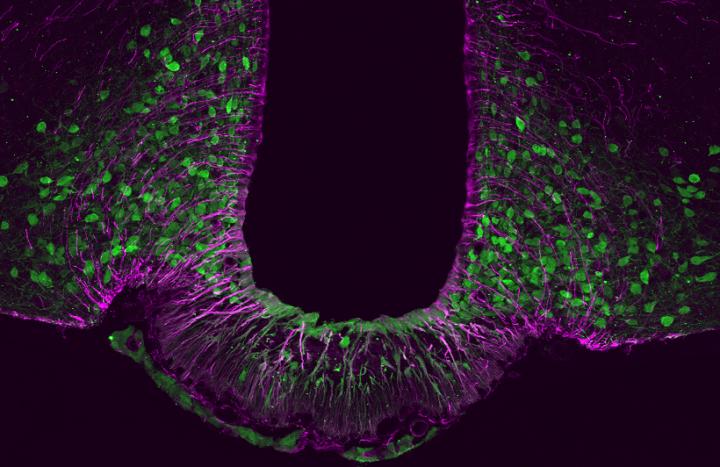
Credit: Source: modified from Quarta, C. & Fisette, A. et al. (Nature Metabolism)
Obesity – as research in the past decade has shown – is first and foremost a brain disease. Researchers at Helmholtz Zentrum München, partners in the German Center for Diabetes Research, have now discovered a molecular switch that controls the function of satiety neurons and therefore body weight. The findings were published in the journal Nature Metabolism.
The worldwide epidemic of obesity has reached record levels, and what was once a problem only of industrialized countries is now also affecting the developing world. Consequently, scientists are working with great commitment to identify the mechanisms underlying the disease in order to find new treatments. Researchers at the Institute of Diabetes and Obesity (IDO) of Helmholtz Zentrum München have recently taken a further step in this direction.
Yin and yang of energy metabolism
“Whether we’re hungry or feel full is largely determined in the brain – specifically in the hypothalamus,” explains IDO scientist Dr. Alexandre Fisette, together with Dr. Carmelo Quarta lead co-authors of the aforementioned paper. “Two groups of neurons in the hypothalamus control body weight and energy balance via various molecular messengers. Like yin and yang, they help strike a good balance.” While neurons known as Agrp increase appetite, their counterparts, Pomc neurons, produce a sensation of satiety. However, if the interplay between the two is disturbed, the result can be obesity or type 2 diabetes.
“In our recent study we discovered that a transcription factor* called Tbx3 plays a key role in this mechanism,” says Carmelo Quarta, describing the new findings. “Specifically, in the absence of Tbx3, the neurons responsible for producing a feeling of satiety are no longer able to synthesize the expected molecular messengers.” Applying a broad range of techniques, the scientists were then able to show that Tbx3 plays a pivotal role in maintaining energy and sugar metabolism.
Lack of Tbx3 leads to an identity crisis
“Both in a preclinical model and in fruit flies, the absence of Tbx3 leads to a kind of identity crisis of satiety neurons, resulting in obesity,” says Alexandre Fisette. The same signaling pathways also appear to be present in humans: “In preliminary experiments with human neurons, we were able to show that they are no longer able to carry out their function in the absence of Tbx3,” Carmelo Quarta adds.
“Humans with genetic defects in the Tbx3 gene have long been reported to suffer from obesity,” explains study director Prof. Dr. Dr. h.c. Matthias H. Tschöp, CEO of Helmholtz Zentrum München and holder of the Chair for Metabolic Diseases at the Technical University of Munich.** “Our study explains for the first time the underlying mechanisms and once again focuses attention on the central role of the brain in regulating energy metabolism. We hope that Tbx3 may come into consideration one day as a target for drug therapies.”
###
Further Information
* Transcription factors are proteins that determine whether or not specific genes are read. They generally achieve this by influencing (promoting or suppressing) the binding of RNA polymerase to the DNA sequence that codes for the corresponding gene. In this case Tbx3 stands for T-box gene 3.
** It has been reported that TBX3 mutations in humans cause a rare genetic disorder called ulnar-mammary syndrome. The syndrome is associated with a number of typical symptoms, including delayed puberty, a lack of growth hormone production and, most notably, obesity.
Background:
The study was conducted in close collaboration with the lab of Claudia Doege at the Columbia University, New York.
Original Publication:
Quarta, C. & Fisette, A. et al. (2019): Functional identity of hypothalamic melanocortin neurons depends on Tbx3. Nature Metabolism, DOI: 10.1038/s42255-018-0028-1
The Helmholtz Zentrum München, the German Research Center for Environmental Health, pursues the goal of developing personalized medical approaches for the prevention and therapy of major common diseases such as diabetes, allergies and lung diseases. To achieve this, it investigates the interaction of genetics, environmental factors and lifestyle. The Helmholtz Zentrum München is headquartered in Neuherberg in the north of Munich and has about 2,300 staff members. It is a member of the Helmholtz Association, a community of 18 scientific-technical and medical-biological research centers with a total of about 37,000 staff members. http://www.
The Institute of Diabetes and Obesity (IDO) studies the diseases of the metabolic syndrome by means of systems biological and translational approaches on the basis of cellular systems, genetically modified mouse models and clinical intervention studies. It seeks to discover new signaling pathways in order to develop innovative therapeutic approaches for the personalized prevention and treatment of obesity, diabetes and their concomitant diseases. IDO is part of the Helmholtz Diabetes Center (HDC). http://www.
The Technical University of Munich (TUM) is one of Europe’s leading research universities, with around 550 professors, 41,000 students, and 10,000 academic and non-academic staff. Its focus areas are the engineering sciences, natural sciences, life sciences and medicine, combined with economic and social sciences. TUM acts as an entrepreneurial university that promotes talents and creates value for society. In that it profits from having strong partners in science and industry. It is represented worldwide with the TUM Asia campus in Singapore as well as offices in Beijing, Brussels, Cairo, Mumbai, San Francisco, and São Paulo. Nobel Prize winners and inventors such as Rudolf Diesel, Carl von Linde, and Rudolf Mößbauer have done research at TUM. In 2006 and 2012 it won recognition as a German “Excellence University.” In international rankings, TUM regularly places among the best universities in Germany. http://www.
The German Center for Diabetes Research (DZD) is a national association that brings together experts in the field of diabetes research and combines basic research, translational research, epidemiology and clinical applications. The aim is to develop novel strategies for personalized prevention and treatment of diabetes. Members are Helmholtz Zentrum München – German Research Center for Environmental Health, the German Diabetes Center in Düsseldorf, the German Institute of Human Nutrition in Potsdam-Rehbrücke, the Paul Langerhans Institute Dresden of the Helmholtz Zentrum München at the University Medical Center Carl Gustav Carus of the TU Dresden and the Institute for Diabetes Research and Metabolic Diseases of the Helmholtz Zentrum München at the Eberhard-Karls-University of Tuebingen together with associated partners at the Universities in Heidelberg, Cologne, Leipzig, Lübeck and Munich. http://www.
Contact for the media:
Department of Communication, Helmholtz Zentrum München – German Research Center for Environmental Health, Ingolstädter Landstr. 1, 85764 Neuherberg – Tel. +49 89 3187 2238 – E-mail: [email protected]
Scientific contact:
Dr. Alexandre Fisette, Helmholtz Zentrum München – German Research Center for Environmental Health, Institute of Diabetes and Obesity, Ingolstädter Landstr. 1, 85764 Neuherberg – Tel. +49 89 3187 1652 – E-mail: [email protected]
Media Contact
Alexandre Fisette
[email protected]
49-893-187-1652
Original Source
https:/
Related Journal Article
http://dx.




