In the high-stakes arena of liver cancer surgery, the ability to predict post-operative complications is not just advantageous—it can be life-saving. A groundbreaking prospective study published in BMC Cancer unveils a pivotal advancement in predicting post-hepatectomy liver failure (PHLF) by focusing on the intraoperative measurement of indocyanine green retention rate at 15 minutes (ICGR15) specifically in the remnant liver. This innovative approach promises to shift the paradigm in hepatic surgery for hepatocellular carcinoma (HCC) patients, providing surgeons with a reliable, real-time indicator to assess patient risk during hemi-hepatectomy procedures.
Post-hepatectomy liver failure remains one of the most vexing and critical complications following liver resection, particularly in cases involving HCC, where the delicate balance between removing cancerous tissue and preserving sufficient liver function is paramount. Historically, preoperative assessments and static post-operative indicators have fallen short in accurately forecasting severe liver failure, leaving clinicians in a precarious position regarding operative decisions and post-surgical management. The study conducted by Liang et al. aims to transcend these limitations by leveraging dynamic intraoperative data tailored to the function of the future liver remnant.
Indocyanine green (ICG) has long been a trusted compound in hepatic diagnostics due to its rapid clearance by healthy liver tissue, making the retention rate an insightful proxy for liver function. The innovation of measuring ICGR15 intraoperatively stems from the insight that liver function dynamically evolves during surgery, especially as portions are resected and the remnant liver assumes greater physiological burden. Detecting how effectively the remaining liver processes ICG provides a real-time functional assessment unmatched by preoperative or postoperative readings alone.
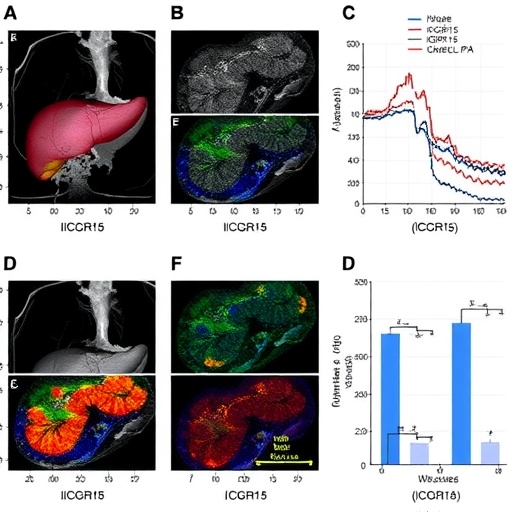
The study’s results were striking: 25.8% of participants developed grade B or C PHLF, categorized as moderate to severe liver failure following the International Study Group of Liver Surgery (ISGLS) standards. Among the three ICGR15 measurements, intraoperative ICGR15 specific to the remnant liver emerged as the most robust predictor of severe PHLF, showcasing a receiver operating characteristic area under the curve (ROC-AUC) of 0.864 and a precision-recall area under the curve (PR-AUC) of 0.791. These statistical indicators highlight the strong discriminatory power of intra-hepatectomy ICGR15 to differentiate between patients at high and low risk of post-surgical liver failure.
A critical threshold for the intraoperative ICGR15 was identified at 19.8%. Patients with a remnant liver ICGR15 equal to or exceeding this value were found to be at a dramatically increased risk of grade B/C PHLF—with an odds ratio of 3.602, underscoring the magnitude of risk elevation. This pivotal finding holds profound clinical implications, as it not only quantifies risk but also furnishes surgeons with actionable data on the operating table. By identifying high-risk patients in real-time, operative strategies can be adapted, and postoperative care intensified, potentially mitigating adverse outcomes.
Complementing conventional logistic regression analyses, the research team employed the cutting-edge XGBoost machine learning algorithm to corroborate their findings and evaluate the relative importance of various predictive parameters. The use of Shapley additive explanations (SHAP values) provided transparency into model decisions, confirming the superior predictive value of intraoperative ICGR15 over pre- and postoperative counterparts. This integration of artificial intelligence exemplifies how modern computational tools can augment clinical insights, refining risk models for greater precision in patient care.
Beyond the immediate context of liver failure prediction, these findings speak to broader surgical oncology strategies. Managing hepatocellular carcinoma requires balancing aggressive tumor resection with preserving adequate hepatic function. The ability to assess remnant liver function intraoperatively addresses a critical gap in surgical planning, potentially reducing the incidence of severe postoperative complications linked to insufficient hepatic reserve.
Furthermore, this study opens avenues for augmented surgical decision-making protocols. Surgeons armed with real-time ICGR15 data may elect to modify the extent of resection, employ tailored perioperative therapies, or institute heightened postoperative monitoring for patients crossing the identified risk threshold. In doing so, the methodology promises not only to improve individual patient outcomes but also to set new standards in hepatic surgery best practices.
It is worth noting that the study’s prospective design and focus on hemi-hepatectomy patients fortify the reliability of its conclusions, although the relatively limited sample size of 31 subjects invites future larger-scale research to validate and possibly expand the applicability of these findings. Nonetheless, the clarity and strength of the data presented offer a compelling argument for adopting intra-hepatectomy ICGR15 assessments as a routine part of surgical liver cancer management.
The clinical implications resonate beyond the operating theater. Hospitals and healthcare systems may leverage these insights to optimize resource allocation—prioritizing intensive care resources for patients identified intraoperatively as high risk, thereby improving overall treatment efficiency and survival rates. Moreover, patients benefit through more personalized surgical counseling, understanding their intraoperative risk profiles better, and engaging in informed consent processes reflecting real-time liver function assessments.
Technical nuances embedded within this research deserve particular attention. Measuring ICGR15 intraoperatively requires precise timing and integration with surgical workflows, ensuring patient safety and accurate data collection without disrupting operative efficiency. The study sets a precedent for more sophisticated intraoperative monitoring techniques, perhaps inspiring parallel innovations in other surgical domains where organ function dynamics critically impact outcomes.
In conclusion, Liang and colleagues have illuminated a crucial path forward in hepatocellular carcinoma surgery by demonstrating the predictive supremacy of intra-hepatectomy ICGR15 for the remnant liver in foreseeing post-hepatectomy liver failure. This advancement epitomizes the convergence of surgical expertise, diagnostic innovation, and artificial intelligence, converging to enhance patient safety and surgical success. As the surgical community continues to wrestle with the complexities of liver cancer treatment, intraoperative functional assessment stands out as a beacon guiding more precise, patient-specific interventions.
As research continues to unfold, the integration of intraoperative ICGR15 measurements into multimodal assessment protocols holds potential to be further enhanced by emerging technologies—such as intraoperative imaging and advanced machine learning models—fortifying the clinical decision-making arsenal against PHLF. The implications are profound: shifting from reactive to proactive surgical management, ultimately translating to saved lives and improved quality of life for patients battling hepatocellular carcinoma.
Subject of Research: Predictive evaluation of intra-hepatectomy indocyanine green retention rate at 15 minutes (ICGR15) for assessing post-hepatectomy liver failure risk in hepatocellular carcinoma patients undergoing hemi-hepatectomy.
Article Title: Predictive value of intra-hepatectomy ICGR15 of the remnant liver for post-hepatectomy liver failure in hemi-hepatectomy: a prospective study
Article References:
Liang, T., He, Y., Mo, S. et al. Predictive value of intra-hepatectomy ICGR15 of the remnant liver for post-hepatectomy liver failure in hemi-hepatectomy: a prospective study. BMC Cancer 25, 881 (2025). https://doi.org/10.1186/s12885-025-14296-5
Image Credits: Scienmag.com
DOI: https://doi.org/10.1186/s12885-025-14296-5
Keywords: post-hepatectomy liver failure, hepatocellular carcinoma, indocyanine green retention rate, intra-hepatectomy monitoring, liver resection, hemi-hepatectomy, predictive modeling, XGBoost, ISGLS criteria
Tags: dynamic intraoperative risk assessmenthemi-hepatectomy procedureshepatocellular carcinoma treatmentindocyanine green retention rateintraoperative measurement in liver surgeryliver cancer surgeryliver function preservation during surgeryliver resection complicationspost-hepatectomy liver failure predictionprospective study on liver failurereal-time indicators in hepatic surgerysurgical outcomes in liver cancer