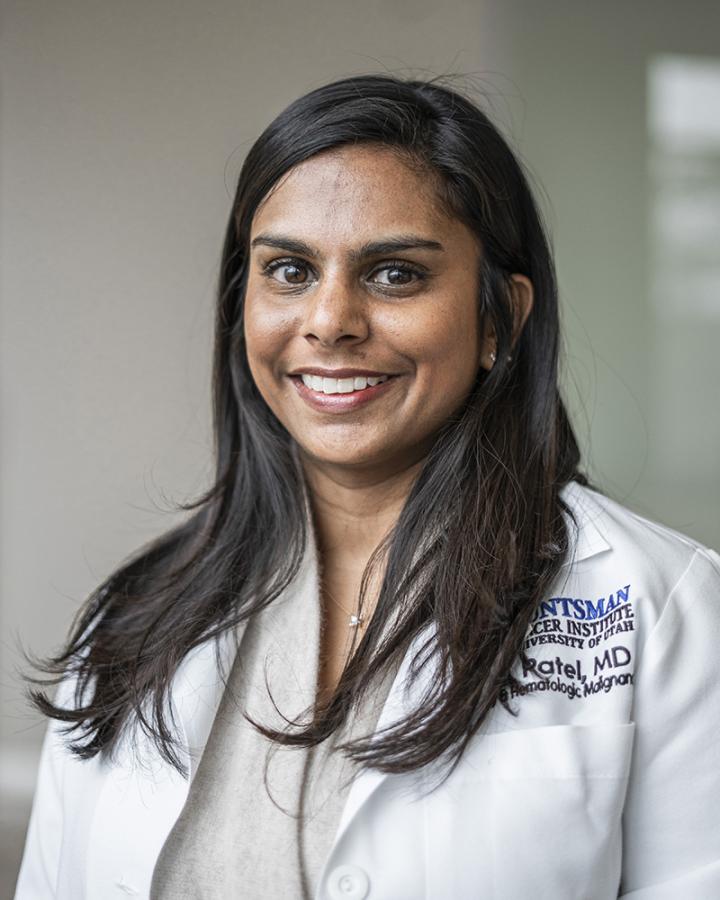
Credit: Huntsman Cancer Institute
Tyrosine kinases are protein enzymes that have many functions within cells, including cell signaling, growth, and division. Sometimes these enzymes can be overactive, which helps cancer cells survive and multiply. A tyrosine kinase inhibitor (TKI) is a medication given to certain acute myeloid leukemia (AML) patients to block the actions of overactive tyrosine kinases, with the ultimate goal of stopping or slowing cancer cell growth. In a study published in the journal Leukemia, lead author Ami Patel, MD, Huntsman Cancer Institute (HCI) researcher and assistant professor in the Division of Hematology and Hematologic Malignancies at the University of Utah (U of U), showed that factors produced by bone marrow support cells allowed leukemia cells to survive treatment with quizartinib, a type of TKI. When quizartinib was combined with another TKI called dasatinib the alternative survival pathways were shut down, leading to more effective leukemia cell death. Patel and colleagues believe this study helps to outline a potential new treatment approach in AML patients who have a mutation in a gene called FLT3.
AML is a type of blood cancer that affects white blood cells in the body. About 30% of all AML patients have a mutation in a tyrosine kinase called FLT3. This protein sits on the surface of blood cells and binds to a specific molecule called FL outside the cell. Normally, binding of FL activates the FLT3 receptor and causes cell growth. However, when mutations occur in FLT3 growth signals are sent to leukemia cells even when FL is not present. Quizartinib is a type of FLT3 inhibitor that was developed for AML patients with FLT3 mutations.
AML patients respond well to quizartinib initially, but usually their disease returns shortly after treatment. “It is amazing to see how small molecule inhibitors have transformed cancer care for so many leukemia patients,” said Patel. “However, the sobering reality is that even new and exciting drugs often only work to control leukemia for a finite period of time before the patient develops drug resistance and relapses.”
Using blood and marrow samples donated by AML patients at HCI, Patel found that factors produced by bone marrow support cells are taken up by leukemia cells, activating survival pathways that protect leukemia cells from being killed by quizartinib. One of the signaling pathways activated in leukemia cells was the STAT5 pathway. Patel also found that these bone marrow factors speed up energy production in leukemia cells, allowing for cancer cell survival. Treating leukemia cells with a combination of quizartinib and dasatinib overcame the protective effects from bone marrow support cells in this laboratory study and killed leukemia cells more effectively than quizartinib alone.
Patel plans to use these findings to support future studies of resistance to TKIs in another type of leukemia called chronic myelomonocytic leukemia. Collectively, insights from these studies will be used to develop clinical trials to improve treatment options for leukemia patients.
###
This study was supported by the National Institutes of Health including the National Cancer Institute (NCI) P30 CA042014, R21 CA20593601, R01 CA178397, the American Society of Hematology Research Training Award for Fellows, the V Foundation for Cancer Research translational research grant T2017-008, and Huntsman Cancer Foundation.
Media Contact
Carley Longhurst
[email protected]