Penn Medicine, University of Leeds findings have implications for new drug targets for lupus, other autoimmune disorders
Credit: Miriam Walden, Leeds University
PHILADELPHIA – BRCA–the family of DNA-repair proteins associated with breast, ovarian prostate, and pancreatic cancers–interacts with a multipart, molecular complex that is also responsible for regulating the immune system. When certain players in this pathway go awry, autoimmune disorders, like lupus, can arise. Now, researchers in the Perelman School of Medicine at the University of Pennsylvania and colleagues at the University of Leeds, United Kingdom, have deciphered the structure of the complex and have found new molecular targets for fighting autoimmunity. Their findings are published this week in Nature.
“The important association between this complex and the immune system originally came about because my lab focuses on how BRCA1/2 function in DNA damage responses, and we realized that immune signaling entailed similar events that are governed by some of the same players involved in BRCA function,” said co-senior author Roger Greenberg, MD, PhD, a professor of Cancer Biology and director of Basic Science at the Basser Center for BRCA.
An enzyme that functions with BRCA1 to repair damaged DNA also exists within a separate complex called BRISC to regulate immune signaling. Greenberg’s team explored the relationship between BRISC and immune cell surface receptors to better understand the symptoms of lupus and other autoimmune diseases.
The overproduction of immune cells, and their signaling compounds called cytokines, stirs up hyper-inflammation that can cause substantial tissue damage, an effect of many autoimmune disorders. Lupus patients, in particular, produce too much of the cytokine interferon, a natural chemical that signals to the immune system in ways that can exacerbate inflammation.
Greenberg collaborated with University of Leeds structural biologist Elton Zeqiraj to figure out the structure of the molecular complex using cryo-electron microscopy (cryo-EM). Their findings revealed a fascinating molecular mechanism that connected BRISC to an enzyme involved in metabolism called serine hydroxymethyltransferase 2 (SHMT2). SHMT2 guides reactions essential for basic body functions, such as building blocks for proteins and DNA, after being activated by a form of vitamin B6.
By probing the detailed structure of the complex, the team found that SHMT2 also induces immune cells to send out cytokines through its interaction with the BRISC complex. Mutations that disrupt the binding area of BRISC-SHMT2 interfere with this onslaught of inflammation, suggesting a new target for a lupus drug. This interaction was also regulated by vitamin B6 levels in cells, providing clues to the impact of metabolism on immune response regulation.
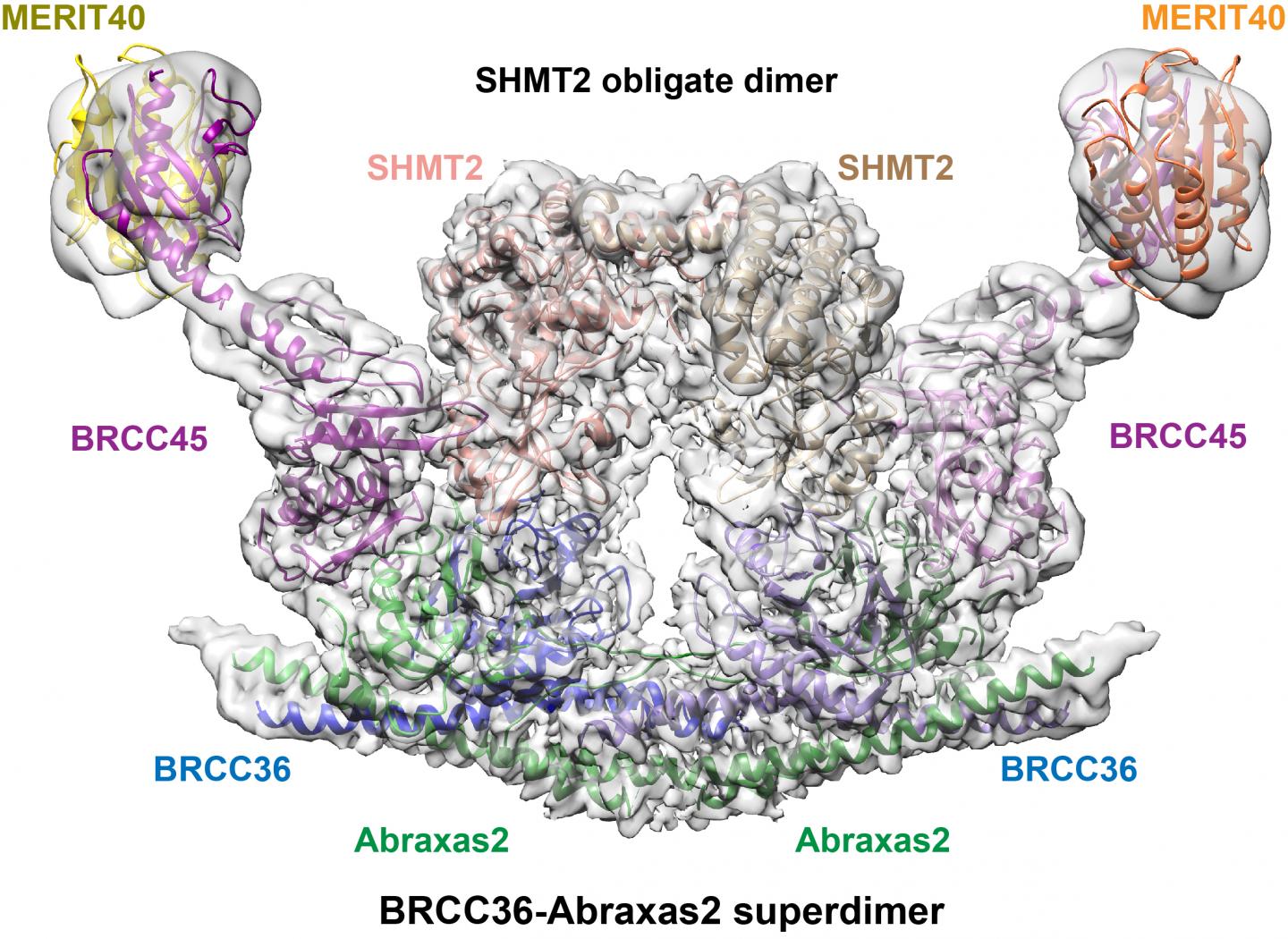
Specifically, the team solved the cryo-EM structure of the human BRISC-SHMT2 molecular complex. They found that it is composed of four BRISC-enzyme protein subunits in a U-shape, with different enzyme components protruding from each side. SHMT2 bridges the gap between the two arms, blocking the active-site pocket, and inhibiting enzyme activity. This block is thought to prevent abnormal BRISC activity and restrict it to inflammatory sites to keep immune signaling in line.
Building on this work, the team plans to explore designing drugs against BRISC in order to quiet overactive cytokine production. “We want to find a drug targeting BRISC to decrease interferon in order to help lupus patients,” said Greenberg. “Knowing the vulnerabilities in the detailed structure of the BRISC-SHMT2 complex gives us new targets to work with.”
Greenberg, Zeqiraj, with medicinal chemist Joseph Salvino of the Wistar Institute, who was also involved in this study, are developing potent small molecule inhibitors of BRISC.
“We have worked together for the past decade, using a multidisciplinary approach to tackle some of the biggest questions in molecular biology,” said Zeqiraj. “Combining our strengths and expertise has led to some very unexpected discoveries, where the end results are better than if we were working alone.”
###
The majority of the work was performed by co-first authors Lei Tian from Penn and Miriam Walden from Leeds. This research was supported in part by a Sir Henry Dale Fellowship from the Wellcome Trust and the Royal Society, the National Cancer Institute (R01 CA138835) and the Lupus Research Alliance.
Penn Medicine is one of the world’s leading academic medical centers, dedicated to the related missions of medical education, biomedical research, and excellence in patient care. Penn Medicine consists of the Raymond and Ruth Perelman School of Medicine at the University of Pennsylvania (founded in 1765 as the nation’s first medical school) and the University of Pennsylvania Health System, which together form a $7.8 billion enterprise.
The Perelman School of Medicine has been ranked among the top medical schools in the United States for more than 20 years, according to U.S. News & World Report’s survey of research-oriented medical schools. The School is consistently among the nation’s top recipients of funding from the National Institutes of Health, with $425 million awarded in the 2018 fiscal year.
The University of Pennsylvania Health System’s patient care facilities include: The Hospital of the University of Pennsylvania and Penn Presbyterian Medical Center–which are recognized as one of the nation’s top “Honor Roll” hospitals by U.S. News & World Report–Chester County Hospital; Lancaster General Health; Penn Medicine Princeton Health; and Pennsylvania Hospital, the nation’s first hospital, founded in 1751. Additional facilities and enterprises include Good Shepherd Penn Partners, Penn Home Care and Hospice Services, Lancaster Behavioral Health Hospital, and Princeton House Behavioral Health, among others.
Penn Medicine is powered by a talented and dedicated workforce of more than 40,000 people. The organization also has alliances with top community health systems across both Southeastern Pennsylvania and Southern New Jersey, creating more options for patients no matter where they live.
Penn Medicine is committed to improving lives and health through a variety of community-based programs and activities. In fiscal year 2018, Penn Medicine provided more than $525 million to benefit our community.
Media Contact
Karen Kreeger
[email protected]




