A study of melanoma cells explains a puzzling response they exhibit to ward off T cell attacks
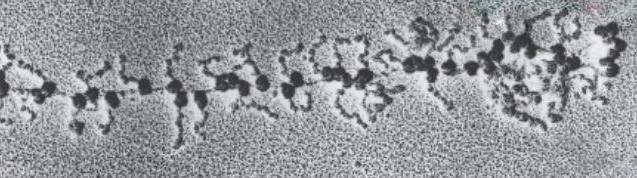
Credit: the Weizmann Institute of Science
Cancers like melanoma are hard to treat, not least because they have a varied bag of tricks for defeating or evading treatments. A combined research effort by scientists at the Weizmann Institute of Science and researchers in the Netherlands Cancer Institute in Amsterdam and the University of Oslo, Norway, shows exactly how tumors, in their battles to survive, will go so far as to starve themselves in order to keep the immune cells that would eradicate them from functioning.
The immunotherapies currently administered for melanomas work by removing obstacles that keep immune cells called T cells from identifying and killing tumor cells. Recent research suggested that in melanoma, another blocker could assist the T cells – this one to stop an enzyme called IDO1 that is overproduced by the cancer cells. IDO1 breaks down an essential amino acid, tryptophan, which is needed to make proteins, in the process leaving behind tryptophan breakdown byproducts that suppress the immune response. But IDO1 blockers did not fare well in clinical trials, suggesting more knowledge was needed – including how the cancer cells, which also require tryptophan, can function after they have destroyed this resource.
The research team, including the group of Prof. Yardena Samuels of Weizmann’s Molecular Cell Biology Department, members of the lab of Prof. Reuven Agami of the Netherlands Cancer Institute; Dr. Noam Stern-Ginossar of the Weizmann Institute’s Molecular Genetics Department; Dr. Yishai Levin and his group at the Nancy and Stephen Grand Israel National Center for Personalized Medicine on the Institute campus; and the group of Prof. Johanna Olweus of the University of Oslo, investigated the mystery of the missing tryptophan in melanoma cells.
Agami and his team had, in previous research shown that in normal cells, when an amino acid like tryptophan is missing, this causes a sort of logjam in the protein production process. The ribosomes – protein production units – make their way down a strand of messenger RNA (mRNA), translating three-letter “words” known as codons into amino acids, which they grab and add to the expanding protein chain. When an amino acid is missing, the ribosomes stop working until one can be found, causing a pile-up in the ribosomes coming up the mRNA strand from behind.
But that is not what happens in melanoma cells. The group found that some ribosomes manage to keep going, past the codons encoding the missing tryptophan. What was going on?
It turned out that the melanoma ribosomes were engaging in a ruse known as “frameshifting.” That is, they simply moved up or down one letter in the RNA strand. In the economical gene code – based on just four letters – the next three spelled the name of a different amino acid and the ribosomes continued down the mRNA strand, assembling protein chains. Of course, the frames of subsequent codon triplets shifted as well, so that the resultant proteins were quite abnormal. The cancer cells then displayed them on their outer membranes, where immune cells could pick up on the aberrant protein structures.
Such frameshifting had been seen before in viruses and bacteria, but not in human cells. Previous studies have missed these proteins because they do not arise from genetic mutations (of which there are hundreds in melanoma), but from a sort of calculated blip in the production process. Agami, whose lab is now investigating exactly how this frameshifting is initiated and whether it occurs in other cancers, says: “This flexibility in mRNA translation might stimulate tumor growth and aggressive behavior by using an emergency program for scarcity.”
Dr. Osnat Bartok, in Samuels’s group: “When things get stressful in the tumor’s microenvironment, it can affect protein production, harming immune cells but also adding to the immune cells’ clues for identifying cancer.” Samuels adds: “These findings add to our knowledge of immune system interactions with cancer as well as the landscape immune cells encounter in a tumor. They suggest exciting ways we might regulate and therapeutically target the presentation of defective immune-reactive peptides on the cell surface.”
###
Dr. Noam Stern-Ginossar’s research is supported by the American Committee for the Weizmann Institute of Science 70th Anniversary Lab; the Ben B. and Joyce E. Eisenberg Foundation; Miel de Botton; and the European Research Council. Dr. Stern-Ginossar is the incumbent of the Skirball Chair in New Scientists.
Prof. Yardena Samuels is Head of EKARD Institute for Cancer Diagnosis Research; and Head of Weizmann-Brazil Tumor Bank. Her research is also supported by the Moross Integrated Cancer Center; the Laboratory in the name of M.E.H Fund established by Margot and Ernst Hamburger; the Green Family Charitable Foundation; the Wagner-Braunsberg Family Melanoma Research Fund; the Jean-Jacques Brunschwig Fund for the Molecular Genetics of Cancer; the Comisaroff Family; the Erica Drake Fund; Miel de Botton; the Hadar Impact Fund; Rising Tide Foundation; the Fundación Ramón Areces; the Hanna and Dr. Ludwik Wallach Cancer Research Fund; the Jacques Asseoff Trust; Karl-Johan Persson; Jean Jacques Roboh; the estate of Adrian Finer; and the European Research Council. Prof. Samuels is the incumbent of the Knell Family Professorial Chair.
The Weizmann Institute of Science in Rehovot, Israel, is one of the world’s top-ranking multidisciplinary research institutions. Noted for its wide-ranging exploration of the natural and exact sciences, the Institute is home to scientists, students, technicians and supporting staff. Institute research efforts include the search for new ways of fighting disease and hunger, examining leading questions in mathematics and computer science, probing the physics of matter and the universe, creating novel materials and developing new strategies for protecting the environment.
Media Contact
Yael Edelman
[email protected]
Original Source
https:/




