High Sodium Intake: A Silent Killer Driving the Global Gastric Cancer Burden
The global health landscape is witnessing an alarming yet often overlooked adversary: high sodium intake. Recent comprehensive research highlights that excessive consumption of sodium significantly contributes to the burden of gastric cancer worldwide. This revelation stems from a thorough epidemiological study analyzing decades of data, revealing that sodium’s impact on cancer mortality is a critical public health concern demanding urgent attention.
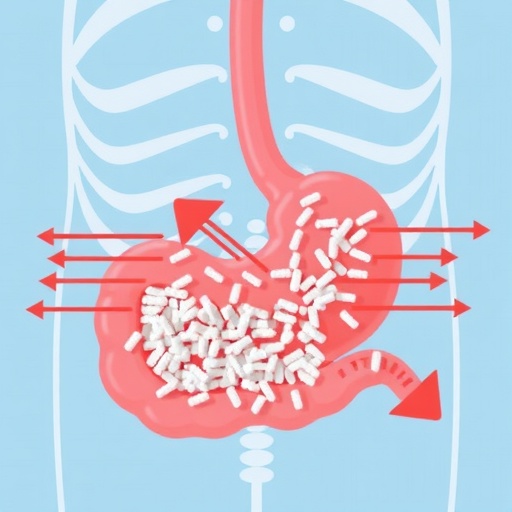
Gastric cancer, one of the leading causes of cancer-related deaths globally, is intricately linked to dietary patterns, with high sodium intake emerging as a major risk factor. Sodium, commonly found in processed and preserved foods, can cause chronic irritation and inflammation of the stomach lining, setting the stage for malignant transformations. The research delves into data spanning from 1990 to 2021, unveiling nuanced patterns of gastric cancer incidence and mortality attributable to sodium consumption.
Utilizing the robust framework of the Global Burden of Disease (GBD) study, researchers applied sophisticated age-period-cohort models to dissect the temporal and demographic factors influencing gastric cancer deaths and disability-adjusted life years (DALYs). This statistical approach allowed for an evaluation of how age groups, temporal periods, and generational birth cohorts contributed variably to disease burden across 204 countries and regions.
In 2021 alone, approximately 7.93% of gastric cancer deaths globally were attributable to high sodium intake, a figure mirroring the 7.92% DALYs linked to this dietary hazard. This proportion underscores sodium’s pervasive role in exacerbating cancer morbidity and mortality, particularly in regions with distinctive sociocultural dietary habits that favor high salt consumption. East Asia and high-middle Sociodemographic Index (SDI) countries emerge as hotspots, bearing the greatest burden of disease linked to excessive sodium.
Despite a concerning prevalence, the study reveals a silver lining: global age-standardized mortality rates and DALYs rates associated with high sodium intake have demonstrated a gradual decline over the past three decades. Net drift analyses indicate an annual percentage decrease of -2.33 for mortality and -2.56 for DALYs. These trends suggest improved public health interventions and awareness campaigns in some regions, particularly those categorized within high SDI brackets, where healthcare infrastructure and regulatory policies have effectively reduced sodium consumption.
China, serving as a pivotal case study within this research, reveals a more complex epidemiological picture. The nation exhibits unfavorable age, period, and cohort effects, with specific age groups and birth cohorts disproportionately affected by high sodium intake’s carcinogenic influence. This pattern highlights challenges in modifying entrenched dietary behaviors and underscores the necessity of more targeted interventions tailored to demographic characteristics.
The pathophysiology that bridges sodium intake and gastric carcinogenesis involves repeated mucosal injury leading to atrophic gastritis, intestinal metaplasia, and ultimately neoplastic transformation. Excessive salt disrupts the gastric mucosal barrier, exacerbates Helicobacter pylori infection risks, and promotes nitrosamine formation—all factors synergizing to elevate cancer risk. These mechanistic insights enrich the epidemiological findings, illustrating a multidimensional attack by sodium on gastric tissue integrity.
Moreover, the study’s projections paint a cautiously optimistic future, suggesting continuing declines in both mortality and DALYs linked to high sodium intake. However, this trajectory depends critically on sustained and enhanced public health strategies to curtail salt consumption globally, especially within high-risk populations. These strategies must integrate culturally sensitive education, policy reforms targeting food industries, and robust surveillance systems.
The gender and age dynamics revealed in the analysis advocate for prioritizing older adults and males in prevention efforts. These subgroups exhibit heightened vulnerability, potentially due to cumulative exposure and behavioral factors affecting sodium intake. Effective communication campaigns should therefore focus on these demographics to maximize impact and reduce the overall gastric cancer burden.
Furthermore, regional variations emphasize the complex interplay between economic development, dietary customs, and health outcomes. East Asia’s heavy burden reflects dietary traditions laden with salted and fermented foods, necessitating nuanced interventions that respect cultural preferences while promoting healthier alternatives. Meanwhile, transitioning economies might face emerging challenges as changing lifestyles and food availability alter sodium consumption patterns.
This comprehensive global assessment underscores the need for international collaboration to combat gastric cancer’s sodium-driven epidemic. Policymakers, healthcare providers, and researchers must synergize efforts to instigate regulatory measures, such as sodium content limits in processed foods and public awareness campaigns, complemented by research into alternative flavoring agents and dietary diversification.
In conclusion, while incremental progress has been made in mitigating gastric cancer’s sodium-associated burden, the findings serve as a clarion call for intensified action. High sodium intake remains a silent killer, disproportionately impacting high-risk regions and populations. By adopting targeted prevention strategies grounded in epidemiological and mechanistic evidence, it is possible to curtail this preventable cause of cancer morbidity and mortality, ultimately safeguarding global health.
Subject of Research: Epidemiological analysis of gastric cancer burden linked to high sodium intake using Global Burden of Disease data and age-period-cohort modeling.
Article Title: High sodium intake: a silent killer driving global gastric cancer burden
Article References:
Zhang, X., Jing, Z., Yu, A. et al. High sodium intake: a silent killer driving global gastric cancer burden. BMC Cancer 25, 1517 (2025). https://doi.org/10.1186/s12885-025-14891-6
Image Credits: Scienmag.com
DOI: https://doi.org/10.1186/s12885-025-14891-6
Keywords: gastric cancer, high sodium intake, Global Burden of Disease, gastric cancer mortality, DALYs, epidemiology, salt consumption, East Asia, Sociodemographic Index, age-period-cohort model
Tags: age-period-cohort models in cancer researchchronic inflammation and stomach liningdietary sodium and cancer preventionepidemiological study on gastric cancergastric cancer incidence and mortalityGlobal Burden of Disease Studyglobal health and dietary patternshigh sodium intake and stomach cancerprocessed foods and health riskspublic health concerns of sodium intakerisk factors for gastric cancersodium consumption and cancer mortality