In a groundbreaking study, a new clinical protocol for postmortem magnetic resonance imaging (MRI) focused on fetal and neonatal cases has been introduced. This protocol is a significant advancement in the field of pediatric radiology and is the result of a concerted effort by the European Society of Paediatric Radiology Postmortem Task Force. This initiative underscores the need for standardized methods in postmortem imaging to enhance both accuracy in diagnostics and the ethical handling of fetal and neonatal cases. In this era of advanced imaging technologies, it is crucial to establish practices that prioritize the well-being of both the patient population and their families.
The study led by D’Hondt, Shelmerdine, and Aertsen highlights the importance of MRI as a non-invasive diagnostic tool in the context of fetal and neonatal deaths. Traditionally, postmortem examinations have relied heavily on autopsies, which, while essential, can be invasive and discomforting for families. The recommendations presented not only aim to reduce the emotional and physical toll on bereaved families but also to improve diagnostic capabilities through state-of-the-art imaging techniques. This dual focus on compassion and medical advancement sets the tone for a new era in pediatric postmortem care.
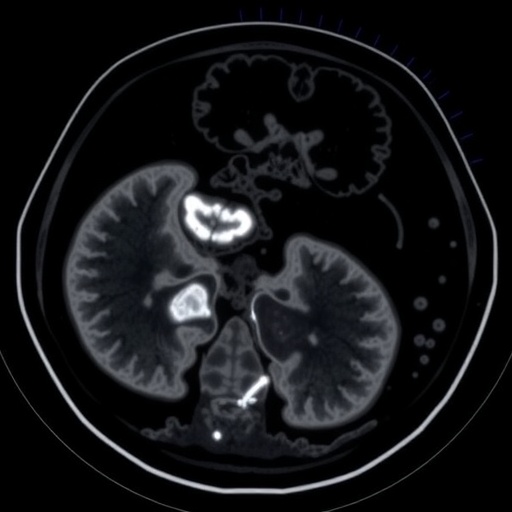
Central to the recommendations is the emphasis on the technical aspects of conducting postmortem MRI scans. The authors recommend specific imaging protocols, including the utilization of high-resolution sequences that can provide detailed insight into congenital anomalies and other pathological changes. These imaging sequences allow for a powerful diagnostic examination, capturing critical information about the condition of the fetus or neonate that may not be visible through traditional methods. The incorporation of advanced imaging software further enhances the interpretative capabilities of healthcare professionals involved in these sensitive cases.
.adsslot_b79RCWtq8j{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_b79RCWtq8j{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_b79RCWtq8j{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
One of the standout features of the proposed protocol is its multidisciplinary approach. It calls for the involvement of pediatric radiologists, neonatologists, and pathologists, who can collaboratively review the imaging results and provide a comprehensive understanding of the circumstances surrounding the death. This teamwork is essential because it brings together different areas of expertise, ensuring that no critical information is overlooked in the evaluation. Such a holistic perspective is vital in understanding the complex interplay of factors that can lead to fetal or neonatal death.
Moreover, the new protocol outlines the importance of obtaining informed consent from families prior to conducting postmortem MRI scans. Given the sensitive nature of this subject, it is crucial that families understand the purpose and potential outcomes of the scans. This transparency fosters trust and ensures that families feel involved in the decision-making process regarding the handling of their loved ones. Communication plays a key role in alleviating the distress families experience during such tragic circumstances.
As technology continues to evolve, the landscape of pediatric imaging will undergo significant transformations. One of the most promising aspects of this new protocol is the incorporation of artificial intelligence (AI) in image analysis. AI can assist radiologists by identifying patterns and anomalies within the scans that may be challenging to detect through the human eye alone. This integration of AI not only enhances diagnostic accuracy but also streamlines the workflow, allowing radiologists to focus on more complex cases that require deeper analytical input.
The authors emphasize that training and education are fundamental in the successful implementation of this new protocol. Specialist training programs should be developed to ensure that pediatric radiologists are not only proficient in MRI technology but also in sensitive communication with grieving families. This dual focus on technical skill and empathetic engagement is critical in ensuring that transitioning to this new protocol enhances both the quality of care and the emotional support provided to families in their time of need.
Ethical considerations are also central to the discussion surrounding the implementation of postmortem imaging protocols. The authors stress the need for a delicate balance between advancing medical knowledge and respecting the dignity of the deceased. They advocate for stringent ethical guidelines to govern the use of postmortem imaging, ensuring that these practices serve to honor the memory of the individuals involved while contributing to the advancement of medical science.
Reassessing standard practices in postmortem care can lead to profound benefits, not only for the families that experience loss but also for medical professionals striving to find answers in difficult cases. The establishment of a standardized protocol as suggested in this recent study encourages communication and consistency in procedures across institutions. Given the diversity of practices currently in place, this uniform approach may help to bridge gaps in experiences for families affected by neonatal and fetal loss.
The transition to utilizing MRI in postmortem examinations reflects a broader trend within medicine towards non-invasive procedures. As engaging in more humane practices takes precedence, the medical community is challenged to reassess traditional methods that may not align with current ethical standards. By broadening the scope of diagnostic tools available, healthcare providers can better comprehend the various factors contributing to fetal and neonatal deaths.
Ultimately, the development of these recommendations signifies a commitment to improving the standard of care within the realm of pediatric postmortem evaluations. By prioritizing the needs of families while maintaining the integrity of medical inquiries, the authors hope to pave the way for future advancements in the field. They believe that this protocol will not only facilitate better clinical outcomes but also foster an atmosphere of compassion and understanding during what is often an incredibly painful time for families.
The groundbreaking work of D’Hondt and colleagues presents an opportunity for pediatric radiology to evolve and adapt to the changing needs of families grappling with loss. By advocating for advancements in imaging and promoting multidisciplinary collaboration, this study lays the foundation for improved practices that will undoubtedly resonate with both families and healthcare professionals alike. The hope is that through rigorous adherence to these recommendations, the intersection of medicine and compassion can lead to better circumstances for those navigating the challenges of neonatal and fetal loss.
Subject of Research: Postmortem Magnetic Resonance Imaging in Fetal and Neonatal Cases
Article Title: Fetal and neonatal postmortem magnetic resonance imaging clinical protocol: recommendations from the European society of paediatric radiology postmortem task force.
Article References: D’Hondt, A., Shelmerdine, S., Aertsen, M. et al. Fetal and neonatal postmortem magnetic resonance imaging clinical protocol: recommendations from the European society of paediatric radiology postmortem task force. Pediatr Radiol (2025). https://doi.org/10.1007/s00247-025-06337-9
Image Credits: AI Generated
DOI: https://doi.org/10.1007/s00247-025-06337-9
Keywords: Postmortem MRI, Fetal Imaging, Neonatal Care, Pediatric Radiology, Ethical Guidelines, Multidisciplinary Approach, Non-Invasive Procedures, Artificial Intelligence in Imaging.
Tags: accuracy in fetal diagnosticsadvancements in imaging technologybereavement support for familiescompassionate medical practicesethical considerations in postmortem careEuropean Society of Paediatric Radiologyfetal and neonatal MRIMRI in neonatal deathsnon-invasive diagnostic techniquespediatric radiology advancementspostmortem imaging guidelinesstandardized postmortem protocols