Recent groundbreaking research published in Molecular Cancer reveals critical insights into the mechanisms of colorectal cancer metastasis, particularly through the actions of a protein called GREM1. The study, led by Zhou and colleagues, investigates the dual role of GREM1 in cancer progression, highlighting a shift from paracrine signaling to autocrine signaling. This transformation plays a significant role in fueling the aggressiveness of colorectal cancer, particularly by activating the Activin receptor-like kinase 1C (ACVR1C). This newly uncovered pathway in cancer biology provides fertile ground for both therapeutic targeting and enhancing our understanding of cancer metastasis.
Colorectal cancer, one of the most prevalent cancers worldwide, poses significant clinical challenges due to its tendency to metastasize. Understanding the intricate molecular pathways involved in cancer spread is essential for the development of effective treatment modalities. This current study addresses a pivotal mechanism previously under-appreciated in the context of tumor biology: the alteration of signaling pathways that can transform how cancer cells interact with their microenvironment. The discovery that GREM1 can shift its signaling mode provides a promising avenue for future research and therapy.
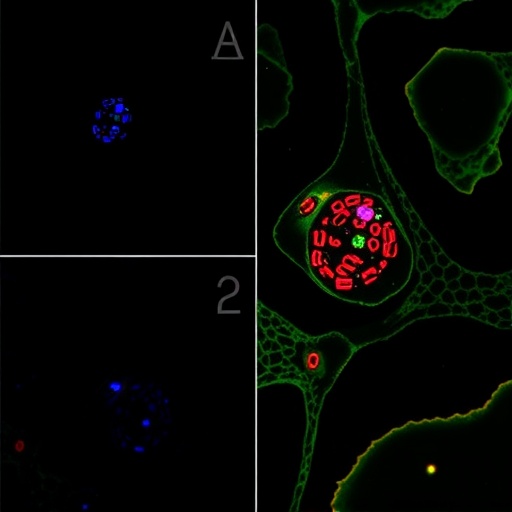
GREM1, short for Gremlin 1, is a bone morphogenetic protein (BMP) antagonist closely associated with various cancers, including colorectal cancer. By blocking BMP signaling, GREM1 plays a role in promoting tumor growth and metastasis. Traditionally thought to act via paracrine signaling—where signals are sent from nearby cells to promote growth—this new study unveils how GREM1 can facilitate its own growth signals through autocrine pathways, where a cancer cell produces signals that act on itself. This switch in signaling type significantly enhances the proliferative capability of cancer cells as they evolve in the tumor microenvironment.
The researchers utilized various experimental models to illustrate the relationship between GREM1 and ACVR1C in colorectal cancer cells. By employing gene editing and pharmacological inhibitors, they demonstrated that inhibiting ACVR1C can significantly reduce the metastatic potential of colorectal cancer cells in vitro. This finding not only underscores the important role of GREM1 in cancer biology but also suggests that therapies targeting this pathway could hold substantial promise for treating patients with advanced colorectal cancer.
Detailed analyses showed that in metastatic colorectal cancer cells, GREM1 upregulates ACVR1C, leading to enhanced cell survival and migration capacities. The study also highlights that the presence of GREM1 alters the transcriptional profile of the cancer cells, promoting gene expressions that are typically involved in cell motility and proliferation. This alteration results in a more aggressive cancer phenotype, which correlates with poorer patient prognosis. Therefore, targeting the GREM1-ACVR1C signaling axis emerges as a groundbreaking approach in therapeutic interventions against colorectal cancer.
Moreover, the research revealed the importance of the tumor microenvironment in influencing the behavior of colorectal cancer cells. The interplay between GREM1 and the surrounding stroma indicates that the tumor is not merely a cluster of malignant cells but rather a dynamic ecosystem. The signaling changes induced by GREM1 can modify the behavior of other surrounding cells, creating an environment that nurtures cancer growth and spread.
One particularly striking aspect of the study is its potential to shift the paradigm in cancer treatment by emphasizing the importance of a dual approach—combining traditional therapies with newer strategies to disrupt this signaling cascade. Current treatment modalities often focus on direct targeting of the tumor cells, but the study highlights that disrupting communication within the tumor microenvironment may be equally important. This holistic view could lead to more effective treatment strategies that address the complex interactions within tumors.
The authors also postulated that the findings could have implications beyond colorectal cancer. Since GREM1 is implicated in several other types of malignancies, understanding its mechanisms could unravel novel intervention strategies across various oncological contexts. By enriching our knowledge of tumor biology, this study contributes to a larger discourse on how cancer therapies might be adapted to more effectively counteract the diverse mechanisms employed by tumors to evade treatment.
In the spirit of this holistic reassessment of cancer dynamics, the research encourages the scientific community to further explore the therapeutic potential of GREM1 inhibition, especially in combinations with existing therapies that target the tumor microenvironment. Future studies that delve deeper into the molecular pathways affected by GREM1 and ACVR1C could yield transformative insights into how to effectively manage advanced cancer cases.
It is crucial to remember that while this research opens new avenues, the path from bench to bedside is multifaceted. Clinical trials will be essential to validate these findings and to understand how best to translate these molecular insights into actionable treatments for patients suffering from colorectal cancer. The authors advocate for an integrated approach that combines targeted therapies with contemporary treatment strategies to improve patient outcomes in the face of this challenging disease.
This research emphasizes the need for continued exploration of the GREM1 signaling pathway, aiming to offer patients not just hope but also practical alternatives in their battle against cancer. The challenges presented by colorectal cancer metastasis are daunting, but with innovative research such as this, there is a significant potential for advancements in both understanding and treatment, which may one day lead to more effective management of this disease.
In conclusion, the findings presented by Zhou and colleagues represent a significant leap in our understanding of colorectal cancer biology. The transition from paracrine to autocrine signaling in GREM1 illustrates a sophisticated level of molecular adaptation that fuels cancer progression. This research not only lays the groundwork for future studies but also encourages a reevaluation of current cancer therapies, emphasizing the importance of addressing tumor microenvironment interactions to combat this pervasive disease more effectively.
Subject of Research: Mechanisms of colorectal cancer metastasis through GREM1 signaling.
Article Title: A paracrine-to-autocrine shunt of GREM1 fuels colorectal cancer metastasis via ACVR1C.
Article References:
Zhou, H., Jin, Q., Fu, Z. et al. A paracrine-to-autocrine shunt of GREM1 fuels colorectal cancer metastasis via ACVR1C. Mol Cancer (2026). https://doi.org/10.1186/s12943-025-02554-w
Image Credits: AI Generated
DOI:
Keywords: GREM1, colorectal cancer, metastasis, ACVR1C, signaling pathways, cancer treatment.
Tags: ACVR1C activation in cancerautocrine signaling in tumorsBMP antagonists in oncologycancer biology research breakthroughscolorectal cancer metastasis mechanismscolorectal cancer treatment challengesGREM1 role in colorectal cancerGremlin 1 and cancer progressionmolecular pathways in cancer spreadparacrine vs autocrine signalingsignaling alterations in tumor microenvironmenttherapeutic targeting of GREM1