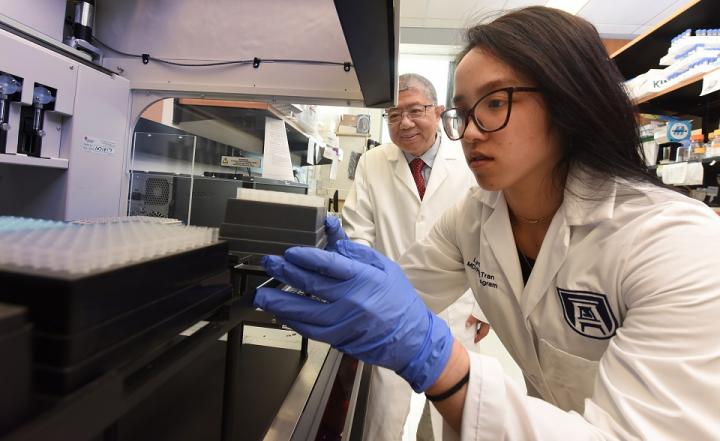
Credit: Phil Jones, Senior Photographer, Augusta University
Women who don’t survive a rare and aggressive uterine cancer called uterine serous carcinoma, have high expression of a group of 73 genes, a score scientists say can help identify these women and improve their outcome.
“It is a very aggressive cancer,” says Lynn Tran, MD/PhD student at the Medical College of Georgia at Augusta University and first author of the study in the journal Gynecologic Oncology.
More than half of women with uterine serous carcinoma, or USC, have more advanced stage 3 or 4 disease at diagnosis and about half the patients who have it die and die very quickly, Tran says. “The question was, can you tell who those half are?”
They found that women with high USC73 scores had the worst prognosis, highest cancer cell proliferation and progression rates, and lowest rates of complete response to standard therapy.
Their findings suggest USC73 score is a biomarker for both the identification of women who will not respond to standard therapy and for efficient clinical trials to find drugs that do work, says Dr. Jin-Xiong She, director of the MCG Center for Biotechnology and Genomic Medicine, Georgia Research Alliance Eminent Scholar in Genomic Medicine and the study’s corresponding author.
Many of these 73 genes have functions important to cancer, like cell survival and migration. When they looked in detail at the cancer cell lines of patients with high expression of what they now call USC73, they found increased cell cycle progression and growth consistent with poor patient survival.
They don’t know yet whether high USC73 is causative of the more aggressive version of this uterine cancer or just associated with it, but are continuing to pursue those answers.
“The difference in survival may be caused by something that we are not measuring, it just may be correlated to the things we are measuring,” Tran says.
The genes they identified have not been consistently reported or described in another cancer but may well be a factor in others, they say, of their signature group.
As next steps, both a retrospective multicenter study, like the work they already have done, and a prospective clinical trial will be conducted to validate the clinical utility of the USC73 gene signature.
“If you can identify the patients who won’t do well and have a very bad prognosis, you can test new drugs on this subset of patients,” She says. “You are going to be able to figure out whether the drug(s) work or not with a much smaller sample size,” a critical factor with such a rare cancer, he notes.
Tran and She say their basic science laboratory assessments can easily be translated to clinical settings with studies done right after surgery and before other therapies, like chemotherapy, begin.
Uterine cancer is generally more common in younger, Caucasian women who have not had children and have obesity. But the rare USC is notorious for affecting non-Caucasian, postmenopausal women who have had children, they say.
To better tailor treatment for these women, accurate predictors of patient survival and response to standard therapy are needed, they write.
So they looked at one of the larger groups of women ever examined with this rare cancer. Their extensive analysis looked at data from 58 patients in the publicly available National Cancer Institute and National Human Genome Research Institute’s Cancer Genome Atlas Program, or TCGA, which includes matched normal samples. They also looked at data on 67 patients at the Georgia Cancer Center.
Genes are comprised of DNA which gets transcribed into RNA, a sort of middle man, which gets translated into proteins, which are a functional unit in the body that makes things happen. To analyze gene expression in these women’s tumors they decided to focus on the middleman RNA, which they can measure more precisely than the end product protein, and consider a more reliable source.
The TCGA data was used to identify the RNA and genes, and their findings held in the Georgia Cancer Center patients.
A high USC73 score was found in 37.9% and 32.8% of the women in the TCGA and Georgia Cancer Center groups, respectively. A few of the genes were at very high levels in the tumors of some patients; in others all the genes were relatively high.
Tumor cells from patients with a high USC73 score proliferated more rapidly both in a laboratory dish and in patients. In fact, the cancer cells of patients with high levels of USC73 grew about twice as fast in the lab, She says.
When they looked at response to treatment, about 90% of patients with low levels of USC73 had a complete response. It was more like 50-50 in those with high levels. They suspect there are subtypes within the known subtype of USC that require a different treatment strategy.
There are ironies in that the pro-proliferative work of these 73 genes should really get the attention of chemotherapy, which is attracted to rapidly dividing cells, but the fact that the carboplatin/paclitaxel regimen doesn’t work in so many women means it may be the wrong chemotherapy, She says. He notes the regimen was adopted from ovarian cancer with little evidence it would be very effective on uterine cancer.
While they don’t know which drugs yet, they think there might be better choices for the nonresponders and already are trying out the effect of other drugs on USC cells in a dish.
They also are looking upstream for master regulator transcription factors that control gene expression to see if at least some can safely be turned off or down, She says.
They note that this group of 73 genes are likely functioning at a low level in a healthy individuals in support of cells with a naturally high turnover rate like skin and hair cells and those that line the gastrointestinal tract.
“Your gut is regenerating, your hair is growing, you want these to be active,” She says. In fact, they have already overexpressed a molecule upstream and cells in a laboratory dish died in response.
The uterus, which sheds its lining monthly during menstruation, is a definite high-cell turnover area so while these genes are active there normally, the scientists selected the 73 suspects on differences between activity in normal and cancerous tissue. “There is a baseline level but we are saying this is much higher,” says Tran.
Endometrial cancer it the most common gynecologic malignancy and over half the deaths are caused by the uncommon subtype USC.
Standard therapy for these women includes surgery, followed by the chemotherapy drugs carboplatin and paclitaxel, and potentially internal or external radiation.
Mutations in a handful of genes have been found in this cancer but trials that target those mutations have not improved survival, the scientists say. Other molecular markers have been identified but not pursued clinically.
The national TCGA has extensive patient data including different molecules in a patient’s tumor, their treatment, how their disease presented in clinic, metastasis and where the cancer spread, and how long they survived, Tran says.
###
Read the full study here.
Media Contact
Toni Baker
[email protected]




