Credit: Copyright 2020 AANS.
CHARLOTTESVILLE, VA (OCTOBER 13, 2020). The authors, two surgeon-researchers from Murayama Medical Center in Tokyo, tested a device that, when attached to everyday eyeglasses, can display fluoroscopic images used for surgical guidance directly to the surgeon. Without such a device, the surgeon must receive this guidance by repeatedly looking across the operating room to a video monitor. The authors found that the eyeglass display device allowed the surgeon to focus on operative tasks more efficiently and resulted in a slightly shorter length of surgery and less exposure to radiation.
Detailed findings of this study can be found in a new article, “Smart glasses display device for fluoroscopically guided minimally invasive spinal instrumentation surgery: a preliminary study,” by Keitaro Matsukawa, MD, PhD, and Yoshiyuki Yato, MD, PhD, published today in the Journal of Neurosurgery: Spine.
An operating room can be a very crowded place. In addition to surgical equipment and personnel, there are numerous intraoperative support systems, including navigation systems that aid the surgeon in performing complicated surgeries. Navigation systems are particularly important when surgery is minimally invasive. However, their placement in the operating room may not be totally convenient to the surgeon.
Fluoroscopy is a form of medical imaging that produces real-time moving X-ray images that visualize a patient’s bone anatomy. In minimally invasive spine surgery, in which the surgical opening is small, fluoroscopy provides the surgeon with a clear view of where and how to affix surgical screws, plates, and other spinal instrumentation.
When fluoroscopy is used, spine surgeons must turn their heads repeatedly to view both the surgical field and the fluoroscopy monitor, which normally stands several feet away from the operating table. This constant movement can be distracting for the surgeon. The authors suggest that it also may cause longer operative times and technical difficulties, and lead to potential errors. The authors hypothesized that wearing a device that displays fluoroscopic images within the surgeon’s visual field during insertion and attachment of spinal instrumentation could improve the safety of minimally invasive spine surgery.
To test their hypothesis, the authors performed a pilot prospective randomized study in 20 patients who underwent posterior lumbar interbody fusion at the L5-S1 spinal level. To the authors’ knowledge, this is the first study on the feasibility of using a wearable display device for fluoroscopically guided, minimally invasive, spinal instrumentation surgery. All surgeries were performed by the same surgeon and, in each case, the percutaneous pedicle screw technique was used.
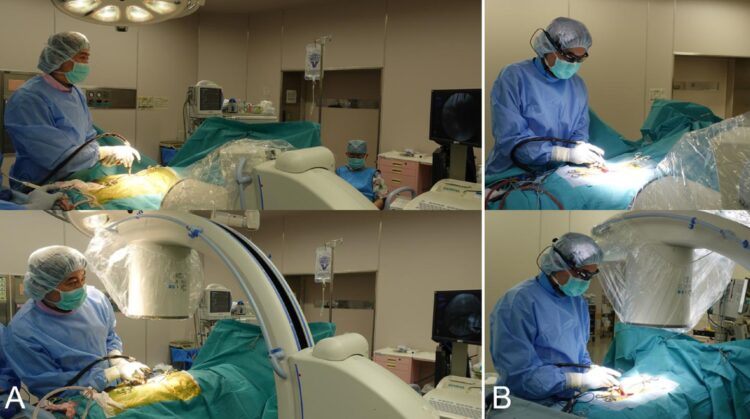
In 10 cases the surgeon wore glasses with an attached device (picoLinker device, Westunitis) that wirelessly displayed real-time fluoroscopic images within the surgeon’s visual field. In the other 10 cases the surgeon wore no display device, but instead frequently consulted the fluoroscopy monitor that was positioned elsewhere in the OR.
To examine whether the wearable display device improved aspects of spine surgery, the authors examined, in each group of patients, the number of times the surgeon’s head turned to consult the fluoroscopic video display, the duration of the operation, and the length of time the patient and surgeon were exposed to radiation emitted by the fluoroscope.
The surgeon turned toward the fluoroscopy monitor significantly fewer times while wearing the eyeglass-attached fluoroscopic display device (means ± standard deviations: 0.1 ± 0.31 vs. 82.4 ± 32.5 times; p
After reviewing the results, the authors conclude that an eyeglass-attached fluoroscopic display device “may be a valid option to enhance the surgeon’s ability to concentrate on operative tasks by improving ergonomic efficiency during surgery.”
When asked about the findings of this study, the authors responded, “We believe the major advantages are ‘concentration’ and ‘information centralization.’ The smart glasses display system used as an alternative screen in front of surgeons’ eyes allows them to see both the surgical field and information displayed on monitors simultaneously without moving the eyes and head. In addition to fluoroscopic images, a variety of other images, such as those obtained before surgery and those from vital sign monitors, neurophysiological monitors, computer navigation monitors, and endoscopic monitors, can be displayed on the wearable screen. The eyeglass-attached display device can be a great tool to help surgery progress smoothly and safely.”
###
Article: Matsukawa K, Yato Y: Smart glasses display device for fluoroscopically guided minimally invasive spinal instrumentation surgery: a preliminary study. J Neurosurg Spine, published ahead of print October 13, 2020. DOI: 10.3171/2020.6.SPINE20644.
Disclosure: Dr. Matsukawa is a consultant for Westunitus, the manufacturer of the picoLinker device.
For additional information, contact: Ms. Jo Ann M. Eliason, Communications Manager, JNS Publishing Group, One Morton Drive, Suite 200, Charlottesville, VA 22903; Email [email protected]; Phone 434-982-1209.
The Journal of Neurosurgery: Spine is a monthly peer-reviewed journal focused on neurosurgical approaches to treatment of diseases and disorders of the spine. It contains a variety of articles, including descriptions of preclinical and clinical research as well as case reports and technical notes. The Journal of Neurosurgery: Spine is one of five journals published by the JNS Publishing Group, the scholarly journal division of the American Association of Neurological Surgeons. Other peer-reviewed journals published by the JNS Publishing Group include the Journal of Neurosurgery, Journal of Neurosurgery: Pediatrics, Neurosurgical Focus, and Neurosurgical Focus: Video. All five journals can be accessed at http://www.
Founded in 1931 as the Harvey Cushing Society, the American Association of Neurological Surgeons (AANS) is a scientific and educational association with more than 10,000 members worldwide. The AANS is dedicated to advancing the specialty of neurological surgery in order to provide the highest quality of neurosurgical care to the public. All active members of the AANS are certified by the American Board of Neurological Surgery, the Royal College of Physicians and Surgeons (Neurosurgery) of Canada, or the Mexican Council of Neurological Surgery, AC. Neurological surgery is the medical specialty concerned with the prevention, diagnosis, treatment, and rehabilitation of disorders that affect the entire nervous system including the brain, spinal column, spinal cord, and peripheral nerves. For more information, visit http://www.
Media Contact
Jo Ann M Eliason
[email protected]
Related Journal Article
http://dx.