In a groundbreaking advance for lung cancer management, researchers have unveiled a dynamic nomogram designed to predict the risk of brain metastasis in patients with stage III non-small cell lung cancer (NSCLC) undergoing definitive chemoradiotherapy. Despite significant strides in extending survival for these patients, brain metastasis remains a dire complication, underscoring the critical need for precise risk stratification methods.
Stage III NSCLC represents an aggressive and heterogeneous disease entity where concurrent chemoradiotherapy is the cornerstone of treatment. While therapeutic protocols have evolved to improve overall survival, the propensity for tumor spread to the brain poses a formidable clinical challenge. Intracranial dissemination drastically compromises neurological function and quality of life, necessitating early detection and preventative interventions.
The study meticulously analyzed a cohort of 311 patients, retrospectively divided into training and validation subsets to rigorously develop and authenticate the predictive model. By integrating univariate and multivariate analyses, augmented with stepwise Akaike information criterion regressions, researchers isolated key independent risk factors for brain metastasis. This meticulous methodology ensured the nomogram’s robust statistical foundation and clinical applicability.
Crucially, the nomogram incorporates a multifaceted panel of predictors, encompassing sex, epidermal growth factor receptor (EGFR) mutation status, presence of liver metastasis, immune maintenance deficiency, neuron-specific enolase levels, carcinoembryonic antigen concentrations, and absolute lymphocyte count. This combination of molecular, immunological, and clinical parameters reflects the complex biology underpinning metastatic dissemination to the brain in NSCLC.
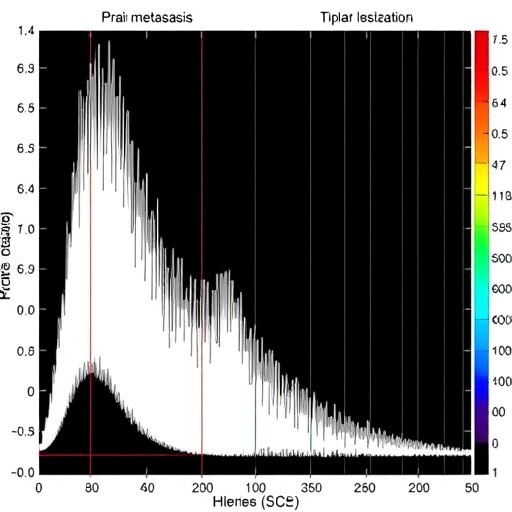
Predictive accuracy was impressive, with the model achieving an area under the receiver operating characteristic curve (AUC) of 0.813 in the training cohort and a commendable 0.775 in external validation. These metrics affirm the nomogram’s superior discriminative power over existing predictive tools, supporting its utility in stratifying patients by metastatic risk with high confidence.
Further validation employed calibration curves and decision curve analysis, confirming the model’s reliability and net clinical benefit. Such rigorous verification affords clinicians a practical instrument to personalize surveillance intensity and therapeutic interventions, potentially enabling preemptive strategies to mitigate brain metastases development.
Survival analyses elucidated the stark prognostic implications of brain metastasis in this patient population. Individuals who developed brain metastases exhibited significantly poorer overall survival—averaging 43.3 months compared to 75.8 months in those without intracranial involvement. This underscores the profound impact of cerebral spread on long-term outcomes and the imperative to identify high-risk patients early.
Remarkably, the researchers established a nomogram-derived cutoff score of 393.79, segmenting patients into high- and low-risk strata. High-risk individuals exhibited markedly shorter median survival, reinforcing the prognostic and clinical significance of the model’s risk categorization. This stratification empowers oncologists to tailor follow-up protocols and consider adjunctive treatments.
The nomogram’s dynamic nature also allows recalibration as new data emerges, fostering adaptability in evolving clinical contexts. By integrating real-world variables such as immune status and tumor markers, this tool encapsulates a holistic cancer profile far beyond traditional staging systems.
From a translational perspective, the implication of biomarkers like neuron-specific enolase and carcinoembryonic antigen suggests avenues for future therapeutic targeting and biomarker discovery. Additionally, the identification of immune maintenance deficiency as a determinant highlights the intricate interplay of host immunity in metastatic progression.
This research represents a significant step forward in precision oncology, bridging the gap between statistical modeling and bedside decision-making. By enabling clinicians to preempt brain metastasis occurrence, patient care can be optimized, and resources can be judiciously allocated toward those most in need of intensive monitoring and early intervention.
In an era where personalized medicine redefines cancer care, predictive models like this nomogram epitomize the convergence of bioinformatics, molecular oncology, and clinical pragmatism. Their integration into routine practice has the potential to transform prognostication, enhance patient counseling, and improve survival outcomes.
Moreover, the availability of this validated tool invites integration with emerging artificial intelligence platforms, potentially enhancing predictive algorithms with machine learning techniques. Future studies may expand upon this framework, incorporating genomic data and longitudinal patient monitoring to refine risk assessments further.
For patients battling stage III NSCLC, this nomogram offers hope through earlier detection of metastatic threats and tailored treatment pathways. By anticipating brain metastasis risk, oncologists can design more proactive strategies, including targeted therapies, stereotactic radiosurgery, or intensified chemoradiotherapy regimens.
Ultimately, this innovative research embodies the future trajectory of oncology: harnessing comprehensive, data-driven tools to anticipate disease progression and improve quality of life. The deployment of such predictive models stands to redefine the frontline management of locally advanced lung cancers in the coming decade.
As research continues to elucidate the molecular underpinnings of metastasis, tools like this dynamic nomogram will be indispensable in translating complex biological insights into actionable clinical strategies, significantly impacting patient survival and well-being.
Subject of Research:
Prediction model development for brain metastasis risk in stage III non-small cell lung cancer patients receiving chemoradiotherapy.
Article Title:
Development and validation of a dynamic nomogram for predicting brain metastasis in stage III NSCLC patients undergoing definitive chemoradiotherapy.
Article References:
Chen, X., Xiao, X., Wang, M. et al. Development and validation of a dynamic nomogram for predicting brain metastasis in stage III NSCLC patients undergoing definitive chemoradiotherapy. BMC Cancer 25, 1500 (2025). https://doi.org/10.1186/s12885-025-14909-z
Image Credits: Scienmag.com
DOI:
https://doi.org/10.1186/s12885-025-14909-z
Tags: advanced lung cancer treatment strategieschemoradiotherapy outcomesdynamic nomogram for brain metastasisEGFR mutation status in NSCLCimmune deficiency and cancer spreadliver metastasis impact on prognosisneurological function in lung cancer patientsNSCLC brain metastasis predictionpredictors of brain metastasisretrospective cohort study in oncologyrisk stratification in lung cancerstage III non-small cell lung cancer