A USF Health preclinical study shows that targeting a promising bitter taste receptor with structurally distinct drugs can help prevent reduced therapeutic effectiveness over time
Credit: Images generated by instrumentation in the Microscopy Core at the University of South Florida Byrd Alzheimer’s Center
TAMPA, Fla. (Oct. 11, 2019) — The waning effectiveness of drugs over time continues to be a major challenge in treating diseases, including asthma.
Half of all patients with moderate-to-severe asthma still fail to achieve optimal control of the inflammatory and airway constrictive components of this chronic disease with currently available drugs. The poorly controlled asthma can lead to shortness of breath, exercise intolerance and hospitalizations.
Aiming to find precise treatments with fewer side effects, Stephen B. Liggett, MD, and colleagues at the University of South Florida Health (USF Health) Morsani College of Medicine examined how distinct structural variations in five drugs (called agonists) might affect their long-term ability to treat airway obstruction. They investigated how each of the five drugs regulated a bitter taste receptor known as TAS2R14 — a G protein-coupled receptor (GPCR) expressed on human airway smooth muscle, deep inside the lungs.
The USF Health preclinical study was published online Aug. 20 in The FASEB Journal.
The current study builds upon previous work by senior author Dr. Liggett, demonstrating that bitter taste receptor agonists appear superior to the inhaled beta-agonists currently prescribed to open airways for asthmatics. In the FASEB paper, the USF Health interdisciplinary research team reports that one drug — diphenhydramine (DPD), a TAS2R14 agonist — worked significantly better than four others to minimize long-term loss of TAS2R14 expression and to maintain the signaling needed to dilate airways over the long term.
“The goal of this study was to see how well the TAS2R14-targeted drugs we selected interacted with the receptor to maintain signaling that relaxes airway smooth muscle — without losing this therapeutic function over time,” said Dr. Liggett, vice dean for research at the USF Health Morsani College of Medicine, and professor of internal medicine and molecular pharmacology and physiology, and medical engineering. “We’re the first to show that it’s possible to bias airway GPCR activation by a drug toward a highly favorable treatment outcome.”
That outcome – improved air flow even with repetitive dosing — indicates the ability to achieve better ongoing control of moderate-to-severe asthma, he added.
“Our portfolio of asthma therapeutics needs drugs that can directly open the airway to treat an acute attack, called rescue drugs, as well as those to prevent attacks, known as controller drugs. But all of these are currently beta-agonists,” Dr. Liggett explained. “We have embarked on finding drugs that activate completely different pathways, so that they can complement or replace current drugs.”
When the effectiveness of a drug diminishes, few options are available, he said. Sometimes a higher dose or more frequent dosing can help, but that can lead to more down-regulation of the response and create a vicious cycle. Accelerated dosing can also cause greater side effects.
GPCRs are cell membrane receptors that receive information from other molecules outside the cell, including drugs. These receptors signal the inside of the cell to carry out one or more functions. In the case of bitter taste receptor TAS2R14, receptor activation triggers the relaxing of constricted airways.
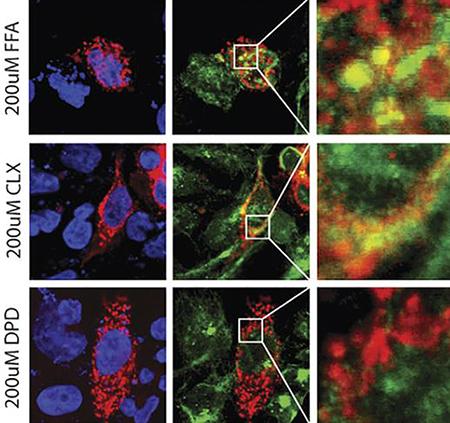
However, with prolonged exposure to a drug, TAS2R14 and many other GPCRs decrease their physiological response to the drug that binds to and activates them. This “desensitization” means that the same dose of drug that originally worked well, no longer does. The process involves a cascade of events — including a reduction in the number of receptors on the targeted cell membrane surface and disrupted cell signaling — all leading to less effective treatment.
The USF Health researchers created a cell model of live human airway smooth muscle cells to study five structurally distinct, existing TAS2R14 agonists including drugs with antiseptic, anti-inflammatory, vessel dilating, and pain-relieving properties. They examined which drugs demonstrated bias away from (did not promote) desensitization of TAS2R14, but still activated this bitter taste receptor.
They also used a computer model known as molecular docking to help identify why the drug DPD interacted with TAS2R14 binding sites differently than most other drugs. Put simply, their docking simulation could predict which key (the drug) best fit into the lock (the receptor pocket) to evoke the special non-desensitizing state of the receptor.
Among some of the study’s key findings:
- – The bitter taste receptor TAS2R14 was exposed to all five drugs for 18 hours. Only DPD showed minimal desensitization after long-term treatment.
– All the drugs except DPD induced the receptors on the surface of airway smooth muscle cells to move into interior of the cell where they eventually are degraded. That leaves fewer receptors on the cell surface to interact with the drug, so the overall treatment response decreases.
– Molecular docking demonstrated that DPD had points of contact deep within the receptor binding pocket not observed with the other four drugs. As a further test, a sixth compound (orphenadrine) structurally similar to DPD was also docked to TAS2R12. Like DPD, orphenadrine conformed to the same contact points on the receptor with no receptor down-regulation. A “best fit” of the agonist into the bitter taste receptor may stabilize the receptor’s shape in a way that promotes optimal drug response, yet avoids down-regulation (and accompanying loss of receptors), the researchers suggest.
Overall, the new research proposes that manipulating the structure of existing drugs or discovering new drugs with structural features that best fit the unique shape of the targeted receptor can promote long-term control of difficult-to-treat asthma, Dr. Liggett said. “It’s like fine-tuning the receptor itself by using the drug to bend it into a shape that works better for the patient.”
###
The USF Health study was funded by grants from the National Heart, Lung and Blood Institute, a part of the National Institutes of Health. The interdisciplinary research involved faculty from Molecular Medicine (Yu Chen, PhD) , Molecular Pharmacology and Physiology (lead author JungA Alexa Woo, PhD), Internal Medicine (senior author Liggett and Donghwa Kim, PhD), and the Microscopy Core at the USF Health Byrd Alzheimer’s Center.
Media Contact
Anne DeLotto Baier
[email protected]
813-974-3303
Related Journal Article
http://dx.




