A worldwide research effort is underway for finding a treatment option for hyperphagia, the most common genetic cause of life-threatening childhood obesity
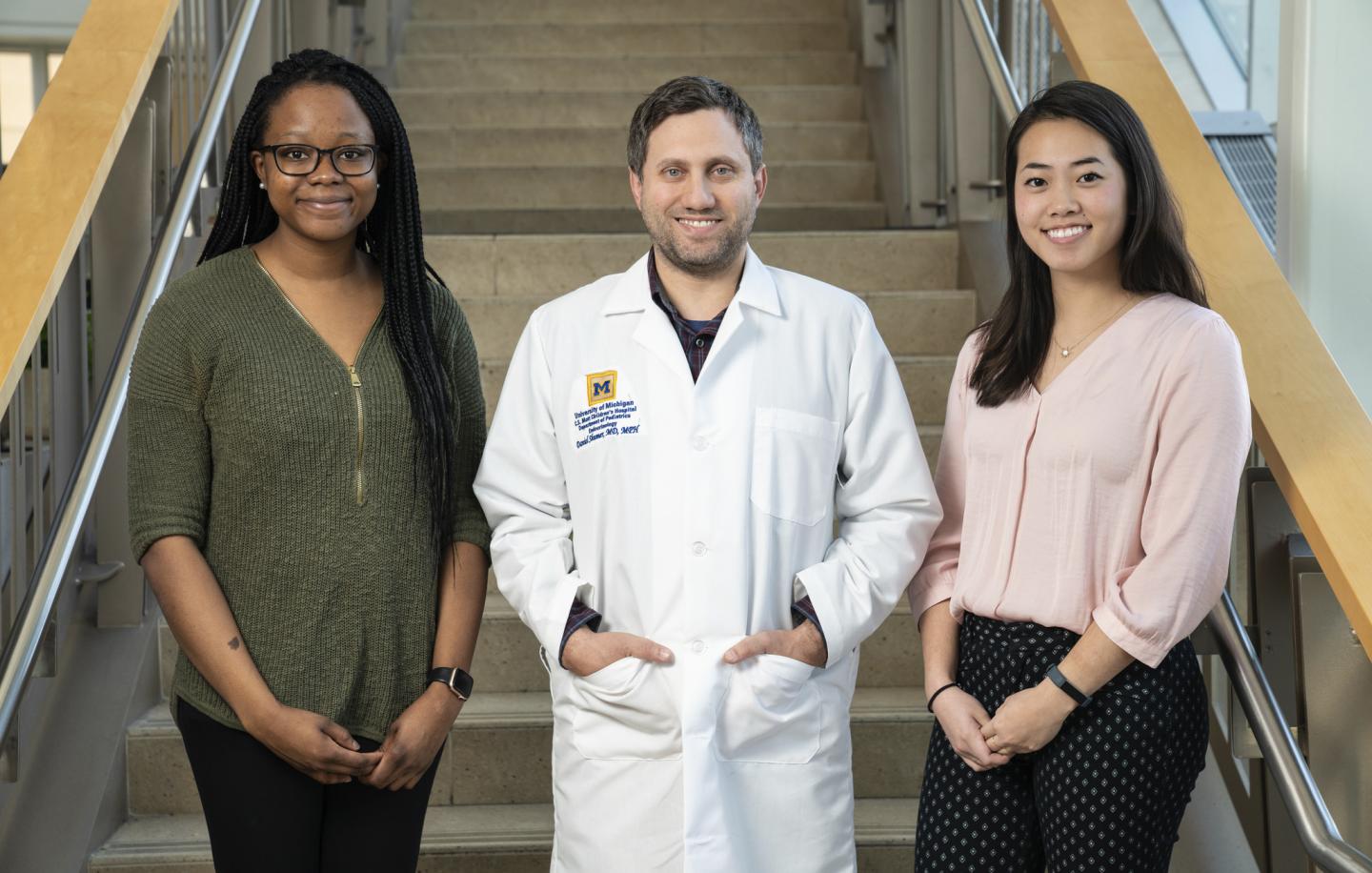
Credit: Michigan Medicine
One in every 15,000 children is affected by Prader-Willi syndrome (PWS), a complex, genetic endocrine condition caused by a disorder of chromosome 15. It’s non-inheritable, meaning the condition isn’t passed down from a family member.
Among the regular side effects like growth hormone deficiency, hypothyroidism, delayed puberty, behavioral problems and learning difficulties, but hyperphagia is regarded as one of the most serious with no current treatment options, according to Daniel Shumer, M.D., pediatric endocrinologist at C.S. Mott Children’s Hospital.
Hyperphagia, an extreme hunger and obsession with food, can result in excessive weight gain in patients with PWS, and is considered the most common genetic cause of life-threatening childhood obesity.
This substantial weight gain can create a domino effect with increased chances of developing diabetes, high blood pressure or hypoventilation.
“This debilitating side effect can provoke children with PWS to raid pantries at home or steal food from school. I know parents that have to put locks on their kitchen cabinets,” says Shumer. “Living with hyperphagia can take a lot of mental energy from the child and those around them.”
PWS, a condition that infrequently gets attention because of its rarity, has researchers around the world looking at the drug Livoletide to reduce the amount of active ghrelin in the brain, a naturally occurring hormone that tells us when we’re hungry.
Millendo Therapeutics, a biopharmaceutical company based in Ann Arbor, is the group tackling the cause.
“Even though this is an international effort with research locations around the country and around the world, Millendo Therapeutics is right in our backyard,” says Shumer. “It’s an Ann Arbor based invention and Michigan Medicine researchers work there. It’s something I’m so proud to be a part of.”
The study, referred to as the ZEPHYR study, was initiated in March 2019 and is a randomized, double-blind placebo-controlled study. When tested in 47 adults who took a three or four milligram dose of livoletide once a day (compared to the placebo) over the course of two weeks, the patients’ health care providers reported a significant decrease in food-related behaviors.
Looking to children with PWS
Now, the researchers are looking to see how children with PWS respond to the drug. Four children are currently enrolled at C.S. Mott Children’s Hospital and recruitment is ongoing for children ages four to seven.
The study not only tests Livoletide’s effectiveness against hyperphagia symptoms, but helps physicians and researchers better understand how the brain works in controlling hunger or experiencing satiety. Better understanding the physiology of the brain has implications for more than just patients with PWS, and could drastically change someone’s quality of life.
“Children with rare diseases are especially vulnerable, since there isn’t a lot of public awareness. When there isn’t awareness there aren’t many treatment options, and that’s isolating for families,” says Shumer. “It’s imperative there are people that work on novel treatments for conditions like this.”
###
Media Contact
Jordyn Imhoff
[email protected]
734-764-2220