A new study led by University of Pittsburgh and UPMC Hillman Cancer Center researchers shows that an enzyme called PARP1 is involved in repair of telomeres, the lengths of DNA that protect the tips of chromosomes, and that impairing this process can lead to telomere shortening and genomic instability that can cause cancer.
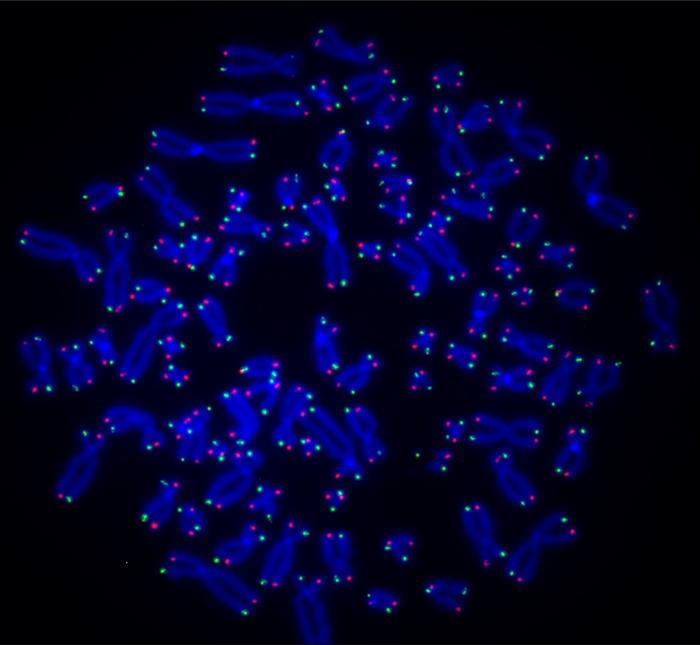
Credit: O’Sullivan Lab
A new study led by University of Pittsburgh and UPMC Hillman Cancer Center researchers shows that an enzyme called PARP1 is involved in repair of telomeres, the lengths of DNA that protect the tips of chromosomes, and that impairing this process can lead to telomere shortening and genomic instability that can cause cancer.
PARP1’s job is genome surveillance: When it senses breaks or lesions in DNA, it adds a molecule called ADP-ribose to specific proteins, which act as a beacon to recruit other proteins that repair the break. The new findings, published today in Nature Structural & Molecular Biology, are the first evidence that PARP1 also acts on telomeric DNA, opening up new avenues for understanding and improving PARP1-inhibiting cancer therapies.
“No one thought that ADP-ribosylation at DNA was possible, but recent findings challenge this dogma,” said Roderick O’Sullivan, Ph.D., associate professor of molecular pharmacology Pitt and investigator at UPMC Hillman. “PARP1 is one of the most important biomedical targets for cancer research, but it was thought that drugs targeting this enzyme only acted at proteins. Now that we know PARP1 also modifies DNA, it changes the game because we can potentially target this aspect of PARP1 biology to improve cancer treatments.”
In normal cells, genomic lesions occur naturally during DNA replication when a cell divides, and PARP1 play an important role in fixing these errors. But while healthy cells have other DNA repair pathways to fall back on, BRCA-deficient cancers — which include many breast and ovarian tumors —rely heavily on PARP1 because they lack BRCA proteins, which control the most effective form of DNA repair called homologous replication.
“When cancer cells can’t make BRCA proteins, they become dependent on repair pathways that PARP1 is involved in,” said O’Sullivan. “So, when you inhibit PARP1 — which is the mechanism of several approved cancer drugs — cancer cells have no repair pathway available, and they die.”
Although scientists discovered PARP1’s role in ADP-ribosylation of proteins about 60 years ago, O’Sullivan and his collaborator, Ivan Ahel, Ph.D., professor in the Sir William Dunn School of Pathology at the University of Oxford and world-renowned expert in PARP1, had a hunch that there was more to learn about this enzyme and its role in cells.
O’Sullivan and his team, led by Anne Wondisford, Ph.D., graduate student in Pitt’s Medical-Scientist Training Program, first compared normal human cells with those deficient in PARP1. Using special antibodies that bind to ADP-ribose and telomere-specific probes, they found that ADP-ribose attaches to telomeric DNA in normal cells but not in PARP1-deficient cells, showing that this enzyme is responsible for ADP-ribosylation of DNA.
Next, they compared normal cells with those deficient in another enzyme called TARG1, which removes ADP-ribose. In absence of TARG1, ADP-ribose accumulated at telomeres, leading to disruption of telomere replication and premature telomere shortening.
To show that these telomere defects were due to modification of telomeric DNA, O’Sullivan and his team took bacterial enzymes that function similarly to PARP1 and put them into human cells.
“We used a guidance system to direct the enzymes to add ADP-ribose only at the telomeres and nowhere else in the genome,” said O’Sullivan. “We found that if we load telomeres with ADP-ribose, their integrity is dramatically impaired, and it can kill the cell within days.”
O’Sullivan hypothesizes that ADP-ribose affects telomere integrity by disrupting a protective structure called shelterin that safeguards telomeres, but more research is needed to confirm this.
“Targeting PARP1 has been a big success story for cancer therapy, but some patients develop resistance to PARP1 inhibitors,” said O’Sullivan. “I’m excited about this study because we’ve discovered something new about PARP1 biology, which generates a whole load of new questions that could help us develop novel approaches to target PARP1 or fine-tune therapies we already have. We’re right at the beginning of something exciting, and there’s a lot more to explore.”
Other authors on the study were Sandra Schamus-Haynes, Ragini Bhargava Ph.D., and Patricia Opresko, Ph.D., all of Pitt and UPMC; Junyeop Lee and Jaewon Min, Ph.D., both of Columbia University; Robert Lu, Ph.D., and Hilda Pickett, Ph.D., both of the University of Sydney; and Marion Schuller, D.Phil., and Josephine Groslambert, both of the University of Oxford.
This research was funded by the National Institutes of Health (R01CA207209, R01262316, P30CA047904, T32 GM133332, F30 CA278287, R35ES030396 and K22CA245259), the Wellcome Trust (101794, 210634, 210634 and 223107), the Ovarian Cancer Research Alliance (813369), Cancer Research UK (C35050/A22284), Medical Research Future Fund (2007488) and the Biotechnology and Biological Sciences Research Council (BB/R007195/1 and BB/W016613/1).
Journal
Nature Structural & Molecular Biology
DOI
10.1038/s41594-024-01279-6
Method of Research
Experimental study
Subject of Research
Cells
Article Title
Deregulated DNA ADP-ribosylation impairs telomere replication
Article Publication Date
7-May-2024


