By identifying a protein that helps regulate blood glucose and lipids, researchers at UNIGE hope for the rapid development of treatments more effective than current insulin therapy
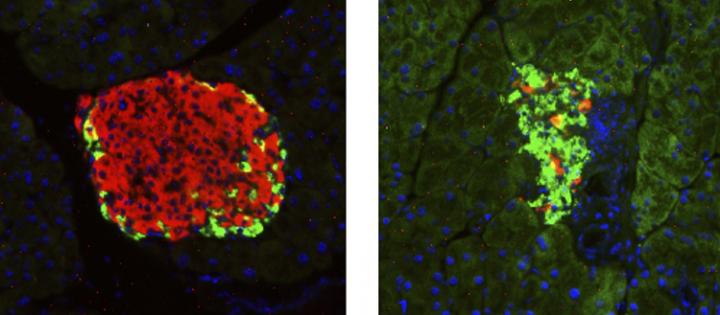
Credit: © UNIGE
Insulin, a hormone essential for regulating blood sugar and lipids, is normally produced by pancreatic β cells. In many people with diabetes, however, pancreatic cells are not (or no longer) functional, causing a chronic and potentially fatal insulin deficiency that can only be controlled through daily insulin injections. However, this approach has serious adverse effects, including an increased risk of life-threatening hypoglycaemia, and it does not restore metabolic balance. In order to improve therapy, researchers at the University of Geneva (UNIGE), Switzerland, have identified a protein called S100A9 which, under certain conditions, seems to act as a blood sugar and lipid regulator while avoiding the most harmful side effects of insulin. This discovery, that can be read in Nature Communications, paves the way for better treatment of diabetes and could significantly improve the quality of life for tens of millions of people affected by insulin deficiency.
Today, insulin injections are essential for the survival of patients with type 1 diabetes or a severe form of type 2 diabetes. However, this treatment is not without risk: overdose can trigger hypoglycaemia, i.e. a drop in blood glucose levels that can lead to coma or even death. But underdosed, it can lead to equally dangerous hyperglycaemia. In addition, insulin is involved in the control of ketones, elements that are produced when the liver breaks down lipids in the absence of sufficient glucose reserves, which become toxic in too large quantities. In addition, long-term insulin treatments cause excess fat and cholesterol in the blood and therefore increases the risk of cardiovascular disease.
As early as 2010, Roberto Coppari’s team, a professor at the Diabetes Centre of the UNIGE Faculty of Medicine, highlighted the gluco- and lipid-regulatory properties of leptin, a hormone involved in hunger control. “However, leptin has proved difficult to use pharmacologically in human beings due to the development of leptin resistance”, says Roberto Coppari. “In order to overcome this problem, we shifted our focus on the metabolic mechanisms triggered by leptin rather than on the hormone itself.”
An effective protein despite its bad reputation
The scientists observed changes in the blood of insulin-deficient mice to whom they administered leptin and noted the abundant presence of the S100A9 protein. “This protein has a bad reputation because, when it binds to its sister protein S100A8, it creates a complex called calprotectin that causes the symptoms of many inflammatory or autoimmune diseases,” says Giorgio Ramadori, a researcher at the Diabetes Centre of the UNIGE Faculty of Medicine and the first author of this work. “However, by over-expressing S100A9, we can, paradoxically, reduce its harmful combination with S100A8, hence dampening calprotectin levels.”
The researchers then administered high doses of S100A9 to their insulin-deficient diabetic mice and found improved glucose management and better control of ketones and of lipids, two metabolic abnormalities that are common in people with insulin deficiency.
In order to better understand how this mechanism translates to human beings, Professor Coppari’s team is currently conducting a clinical observation study, in collaboration with the Geneva University Hospitals, in patients with type 1 and type 2 diabetes presenting very high glucose and ketones levels. They want to identify the correlations between the level of S100A9 in the blood and the severity of symptoms. “In human beings, previous studies already indicated that increased S100A9 levels correlate with reduced diabetes risks; hence, these results further bolster the clinical relevance of our data. As such, we are currently working to progress to phase I human clinical trials to directly test the safety and efficacy of S100A9 in insulin deficiency”, says Roberto Coppari.
Towards combined treatments
The team then made a second discovery: S100A9 protein only appears to work in the presence of TLR4, a receptor located on the membrane of certain cells, including adipocytes or immune system cells. “Why? For the moment, it remains mysterious”, says Roberto Coppari. The researchers are currently working on a treatment that would combine low doses of insulin and S100A9 to better control glucose and ketones and limit high-dose insulin side effects. “We also want to decipher the exact role of TLR4 in order to offer a therapeutic strategy that achieves the delicate balance of optimal blood glucose, ketone and lipid control.”
The stakes are high: tens of millions of people take insulin every day throughout their lives, a treatment that is often difficult to balance for both patients and caregivers. The new therapeutic strategy proposed by Roberto Coppari and his team could greatly improve their quality of life.
###
This work was supported by European Commission, the Swiss National Science Foundation, the Swiss Cancer League, the Louis-Jeantet Foundation, the Fondation Pour Recherches Medicales of the University of Geneva, the Bo and Kerstin Hjelt Foundation for Diabetes Research and the Gertrude Von Meissner Foundation.
Media Contact
Roberto Coppari
[email protected]
41-223-795-539
Related Journal Article
http://dx.




