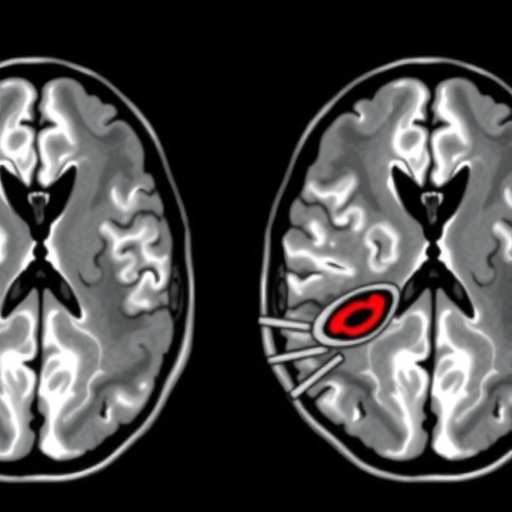
In an era where technology and medicine converge, a groundbreaking study has emerged focusing on the detection and grading of periventricular-intraventricular hemorrhage (PIVH) through advanced cranial ultrasound imaging leveraging deep learning algorithms. Published in the forthcoming issue of Pediatric Radiology, this research spearheaded by Peng et al. from multiple institutions exemplifies the growing capabilities of artificial intelligence in enhancing medical diagnostics. The implications of their findings are profound, potentially transforming how pediatric care is approached, particularly among premature infants who are most at risk of developing PIVH.
Cranial ultrasound has long been a staple in neonatal intensive care units for monitoring brain conditions in newborns. However, the manual assessment of ultrasound images can be both time-consuming and subjective, often leading to variability in diagnoses. The study addresses this challenge by proposing a novel deep learning model designed to analyze ultrasound images more efficiently than traditional methods. By automating the process, the researchers aim to mitigate human error and provide quicker, more accurate assessments.
The research team applied advanced machine learning techniques to develop a convolutional neural network (CNN) specifically catered to analyze cranial ultrasound images. This approach is particularly advantageous due to CNN’s proficiency in recognizing patterns and features within image data. The model was trained using a substantial dataset comprised of images collected from two different centers, allowing it to learn diverse characteristics associated with PIVH across varied populations.
.adsslot_MzaTtIO8HS{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_MzaTtIO8HS{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_MzaTtIO8HS{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
The validation process of the deep learning model was robust and meticulous. Researchers conducted extensive testing to ensure the model’s reliability and accuracy. The results indicated a remarkable performance, with the algorithm achieving a significant reduction in false negatives and false positives when detecting PIVH compared to the standard practices employed in neonatal care. Not only does this enhance diagnostic confidence among clinicians, but it also supports timely intervention, which is critical in managing the health of at-risk infants.
Additionally, the study outlined how the model is capable of grading the severity of hemorrhage, which is essential for guiding treatment decisions. Hemorrhages can vary significantly in severity, and early identification of critical cases can be life-saving. The ability to stratify hemorrhage levels using a standardized, automated system opens the door for tailored treatment plans that can adapt quickly as a patient’s condition evolves.
The implications of this research extend beyond merely improving diagnostic accuracy. By reducing the workload on neonatal healthcare providers, the model allows clinicians to focus more on direct patient care. This paradigm shift could improve outcomes by enabling healthcare professionals to respond more promptly to critical conditions that arise in the NICU environment. The potential for increased efficiency in a high-stakes setting shines a light on how technology can help bridge gaps in healthcare delivery.
Another compelling aspect of the study is its emphasis on the importance of collaboration across institutions. The multicenter approach not only enriched the dataset used for training the deep learning model but also provided a diverse clinical perspective that underscores the model’s generalizability. It demonstrates how collaborative efforts in research can yield more robust and impactful findings, ultimately benefiting patients on a broader scale.
As healthcare systems increasingly integrate technology into their operational frameworks, this study serves as a reminder of the essential ethical considerations that come with it. Developing AI systems in medical contexts must be approached with caution, ensuring that patient safety and data integrity are prioritized at all times. The methodology employed in this research reflects a commitment to responsible innovation, paving the way for future advancements in medical AI.
Looking ahead, the authors anticipate that ongoing developments in machine learning and image processing will further enhance the capabilities of their model. They suggest that future iterations may incorporate additional features, such as real-time image analysis and direct integration with electronic health records to streamline workflows even further. This vision aligns with the broader movement towards personalized medicine where patient-specific data drives clinical decisions.
Moreover, the findings of this study have the potential to inspire further research into the application of AI in other areas of neonatal care beyond just PIVH detection. For instance, similar methodologies could be adapted to evaluate different brain injuries or diseases common among premature infants. The possibilities are vast, indicating a fertile ground for innovative research that could redefine how neonatal conditions are diagnosed and treated.
In conclusion, Peng et al.’s work represents a significant stride toward integrating advanced technologies in routine neonatal care. The development and validation of a deep learning model for cranial ultrasound imaging not only promises increased accuracy in detecting PIVH but could also revolutionize clinical practices in pediatric radiology. The potential benefits to patient outcomes and healthcare efficiency mark a noteworthy milestone in bridging the gap between technology and medicine, encouraging further explorations into AI-assisted healthcare solutions for vulnerable populations.
As the healthcare landscape continues to evolve with technological advancements, studies like this will play a pivotal role in shaping the future of pediatric care. The integration of deep learning into ultrasonic imaging exemplifies the transformative power of AI, setting the stage for ongoing innovation in the fields of radiology and neonatal medicine. This study undoubtedly adds to the burgeoning body of evidence that supports the implementation of machine learning technologies in clinical settings, heralding a new era of medical diagnostics that prioritizes efficiency, accuracy, and patient outcomes.
Subject of Research: Automated detection and grading of periventricular-intraventricular hemorrhage using deep learning in cranial ultrasound imaging.
Article Title: Development and validation of a cranial ultrasound imaging-based deep learning model for periventricular-intraventricular haemorrhage detection and grading: a two-centre study.
Article References:
Peng, Y., Hu, Z., Wen, M. et al. Development and validation of a cranial ultrasound imaging-based deep learning model for periventricular-intraventricular haemorrhage detection and grading: a two-centre study. Pediatr Radiol (2025). https://doi.org/10.1007/s00247-025-06327-x
Image Credits: AI Generated
DOI: https://doi.org/10.1007/s00247-025-06327-x
Keywords: Deep learning, cranial ultrasound, periventricular-intraventricular hemorrhage, pediatric radiology, machine learning, neonatal care.
Tags: artificial intelligence in pediatric medicineautomated image analysis in medicineconvolutional neural networks in diagnosticscranial ultrasound technologydeep learning in medical imagingdetecting periventricular-intraventricular hemorrhageenhancing ultrasound image assessmentmachine learning for healthcareneonatal care innovationspediatric radiology advancementspremature infants and brain healthreducing human error in diagnoses