In recent years, the enigmatic realm of sleep disorders has revealed a fascinating intersection with neurodegenerative diseases, unlocking new pathways for early diagnosis and intervention. Among these disorders, isolated rapid eye movement (REM) sleep behavior disorder (iRBD) has emerged as a compelling harbinger of Parkinsonian syndromes, triggering intense scientific investigation into its neurobiological underpinnings. A groundbreaking study recently published in npj Parkinson’s Disease by Pardo, Roura, Montal, and colleagues pioneers this exploration by meticulously characterizing the cortical macro- and microstructural changes associated with iRBD, providing unprecedented insights into the early neuroanatomical signals preceding overt neurodegeneration.
The phenomenon of REM sleep behavior disorder disrupts the typical paralysis that occurs during the REM phase of sleep, leading to dream enactment behaviors that can range from mild thrashing to violent movements. When this behavior presents in isolation, devoid of comorbid neurological conditions, it serves as a prodromal marker for alpha-synucleinopathies such as Parkinson’s disease (PD) and dementia with Lewy bodies. The challenge for neuroscientists has been to delineate the structural brain alterations in this preclinical stage, potentially allowing for earlier diagnosis, prognostication, and even targeted therapeutic strategies.
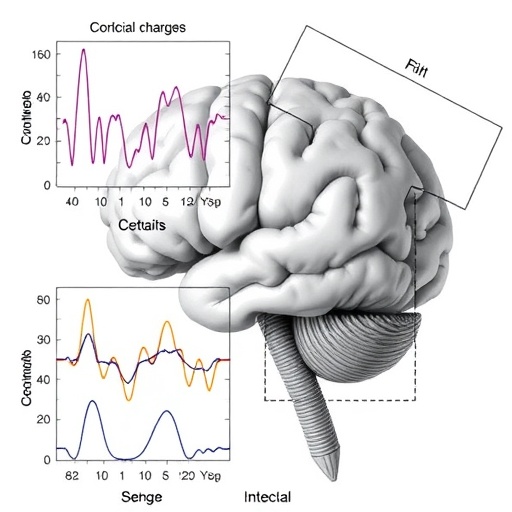
Utilizing state-of-the-art neuroimaging modalities combined with sophisticated computational neuroanatomical analyses, the research team meticulously mapped both macroscopic and microscopic cortical alterations in individuals diagnosed with iRBD. Their approach incorporated advanced diffusion MRI techniques sensitive to microstructural integrity and high-resolution structural MRI for cortical thickness assessment, thereby bridging the gap between gross anatomical changes and subtle cytoarchitectural disruptions.
.adsslot_lCFM3ogpbi{ width:728px !important; height:90px !important; }
@media (max-width:1199px) { .adsslot_lCFM3ogpbi{ width:468px !important; height:60px !important; } }
@media (max-width:767px) { .adsslot_lCFM3ogpbi{ width:320px !important; height:50px !important; } }
ADVERTISEMENT
One of the study’s most striking findings is the identification of widespread cortical thinning in regions implicated in motor control, sensory processing, and executive function. This macroscale cortical atrophy pattern suggests that neurodegenerative processes begin insidiously, even before the emergence of classic motor symptoms that define Parkinsonian syndromes. Importantly, the distribution of cortical abnormalities closely mirrors areas known to accumulate alpha-synuclein aggregates, providing a direct neuroanatomical correlate to underlying molecular pathology.
At the microscale, the researchers detected alterations in tissue microstructure indicative of compromised neuronal and glial integrity. Metrics derived from diffusion tensor imaging (DTI) and neurite orientation dispersion and density imaging (NODDI) revealed decreased neurite density and increased tissue diffusivity in specific cortical layers. Such findings imply early synaptic and dendritic degeneration, preceding significant neuronal loss and reflecting nascent neurodegeneration that may be clinically silent yet biologically significant.
The implications of these microstructural changes extend far beyond mere anatomical curiosity. They offer a window into the pathophysiological cascade that transforms a seemingly benign sleep disorder into a fulminant neurodegenerative disease. By identifying these changes, clinicians and researchers may harness imaging biomarkers to stratify patients at highest risk for progression to Parkinson’s disease, enabling timely therapeutic interventions aimed at neuroprotection or disease modification.
Moreover, the study underscores the heterogeneity of cortical involvement in iRBD, challenging the traditional notion that subcortical structures are the sole initial sites of pathology. The presence of cortical abnormalities suggests a more distributed network degeneration from the earliest stages, encompassing not only movement-related circuits but also cognitive and sensory pathways. This multifocal involvement may explain the diverse prodromal symptoms observed clinically, including subtle cognitive decline, mood disturbances, and impaired sensory integration.
Intriguingly, the research also posits a potential mechanistic link between sleep-related dysfunction and cortical neurodegeneration. Given that REM sleep is critical for synaptic plasticity, memory consolidation, and neuronal homeostasis, disruptions inherent in iRBD may exacerbate or even accelerate cortical vulnerability. This bidirectional relationship opens new avenues for investigating whether interventions targeting sleep architecture could modify disease trajectory.
From a methodological perspective, the study’s integration of multimodal imaging with rigorous quantitative analyses sets a new standard in neurodegenerative research. The application of cutting-edge imaging techniques ensures sensitivity to detect subtle changes that traditional MRI might overlook. Additionally, the use of sophisticated statistical models to correlate imaging metrics with clinical features enhances the translational relevance, bridging bench research with bedside utility.
Further supporting this narrative, longitudinal follow-ups included in the study reinforce the prognostic value of identified cortical changes. Participants exhibiting more pronounced cortical thinning and microstructural disruption at baseline were more likely to develop clinical Parkinsonism during the observation period. This temporal association bolsters the argument for these imaging markers as early predictors, potentially guiding patient counseling and therapeutic decision-making.
The study’s revelations also invite a reevaluation of therapeutic targets in the preclinical stages of synucleinopathies. Traditionally, dopaminergic pathways have been the focus of symptomatic treatment in Parkinson’s disease. However, detecting early cortical involvement suggests that treatments aimed at preserving cortical integrity, modulating synaptic connectivity, or ameliorating neuroinflammation might be critical adjuncts in halting or delaying disease onset.
As the global burden of Parkinsonian disorders continues to escalate with aging populations, the importance of early detection cannot be overstated. The pioneering work by Pardo and colleagues illuminates a critical early window during which neurodegeneration is detectable yet potentially modifiable. It also empowers clinicians with novel biomarker tools, paving the way for precision medicine approaches tailored to individual risk profiles identified through advanced neuroimaging.
Beyond its clinical ramifications, the research enriches the fundamental understanding of neurodegenerative disease pathogenesis. By unraveling the early cortical changes accompanying iRBD, the study challenges existing paradigms and encourages the integration of sleep science, neuroimaging, neuropathology, and clinical neurology into cohesive investigative frameworks.
Future studies building upon these findings are poised to explore mechanistic underpinnings at molecular and cellular levels, potentially combining imaging with cerebrospinal fluid biomarkers, genetic profiling, and electrophysiological assessments. This multimodal approach promises a comprehensive elucidation of disease progression from prodromal sleep disturbances to symptomatic neurodegeneration.
In the realm of public health, these insights emphasize the critical need for heightened awareness of iRBD as a clinical entity warranting diagnostic evaluation and monitoring. Sleep clinicians, neurologists, and primary care providers must recognize the prognostic significance of REM sleep behavioral abnormalities, fostering interdisciplinary collaboration for optimized patient outcomes.
The transformative potential of this research lies not only in its scientific elegance but also in its capacity to affect real-world patient care. By advancing knowledge of early cortical alterations in iRBD, the study provides a compelling roadmap toward early intervention strategies, personalized medicine, and ultimately, improved quality of life for individuals at risk of Parkinsonian neurodegeneration.
In summary, the study “Cortical macro- and microstructural changes in isolated rapid eye movement sleep behavior disorder” deftly elucidates the neuroanatomical landscape of a prodromal stage in Parkinson’s disease. Through sophisticated imaging and analysis, the authors reveal a multifaceted pattern of cortical atrophy and microstructural disruption that anticipates clinical symptomatology. These findings herald a new era of biomarker-driven research and clinical practice, holding promise for breaking the formidable barriers to early detection and intervention in Parkinson’s disease and related synucleinopathies.
Subject of Research: Neuroanatomical and microstructural cortical changes in isolated rapid eye movement sleep behavior disorder as a prodromal marker for Parkinson’s disease.
Article Title: Cortical macro- and microstructural changes in isolated rapid eye movement sleep behavior disorder.
Article References:
Pardo, J., Roura, I., Montal, V. et al. Cortical macro- and microstructural changes in isolated rapid eye movement sleep behavior disorder.
npj Parkinsons Dis. 11, 199 (2025). https://doi.org/10.1038/s41531-025-01058-0
Image Credits: AI Generated
Tags: alpha-synucleinopathies and REM sleepbrain alterations in REM sleep disorderscomputational neuroanatomical analysiscortical changes in sleep disordersisolated REM sleep behavior disorderneuroanatomical signals in iRBDNeurodegenerative Disease Early Diagnosisneuroimaging in sleep researchParkinsonian syndromes and sleepprodromal markers for Parkinson’s diseaserapid eye movement sleep behaviortherapeutic strategies for iRBD