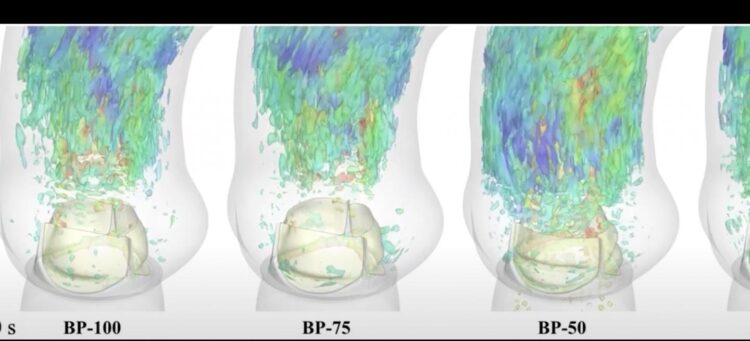
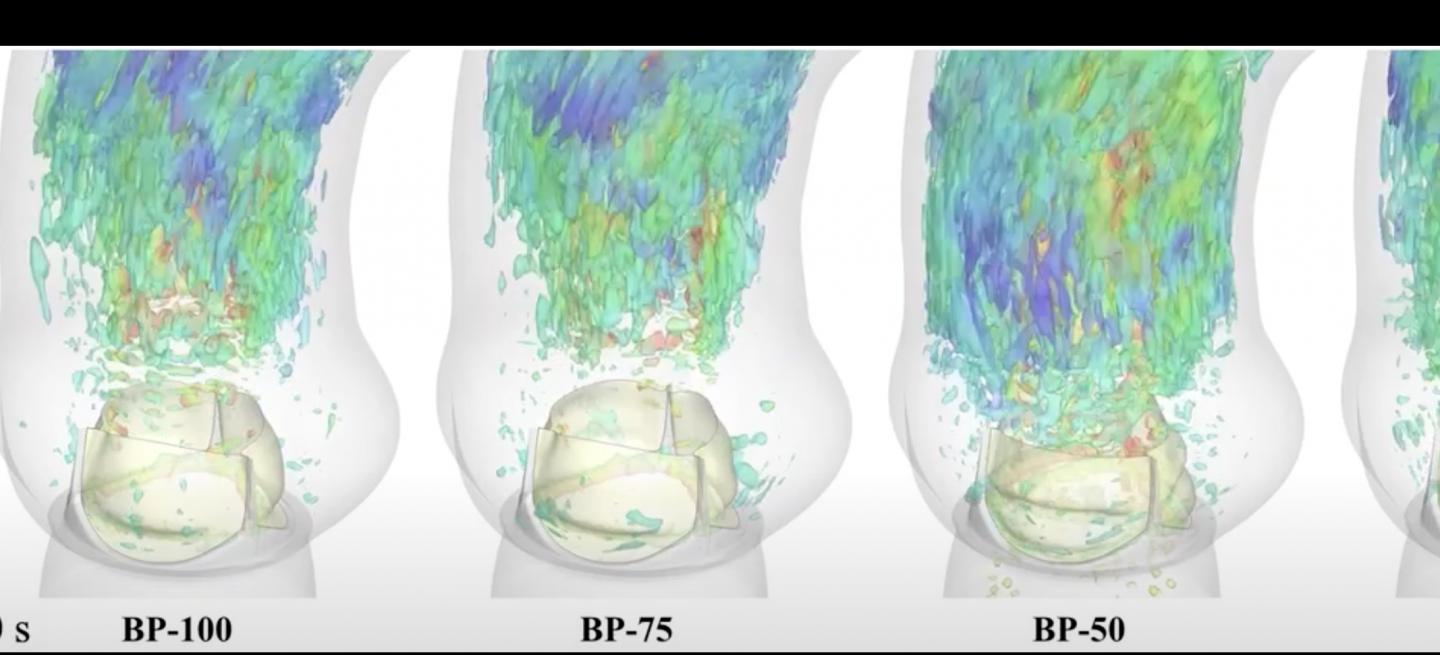
Computational modeling techniques enable unprecedented visualizations of heart valve implant behavior
Credit: Emily L. Johnson.
Computational modeling has provided new insights into the heart’s vascular system, a complex and mechanically demanding system that remains poorly understood.
Researchers from the Oden Institute for Computational Engineering and Sciences at the University of Texas at Austin and Iowa State University used computational modeling techniques to enable accurate visualizations of valve behavior for the first time.
The research was featured in the most recent edition of the journal, PNAS, in a paper entitled: Thinner biological tissues induce leaflet flutter in aortic heart valve replacements.
Valvular heart disease is a growing public health concern due to the high prevalence of valve degeneration among aging populations.
“In the past, valve replacement meant undergoing open-chest surgery, a complex procedure and substantial recovery time,” said Dr. Michael Sacks from the Oden Institute and the Cockrell School’s Department of Biomedical Engineering who coauthored the study with fellow Oden Institute faculty member from Aerospace Engineering and Engineering Mechanics, Dr. Thomas J.R. Hughes. The study’s lead author was Emily L. Johnson from Iowa State University and included other Iowa State colleagues including Oden Institute alumnus, Dr. Ming-Chen Hsu.
Thankfully, many patients with severely diseased aortic valves that need to be replaced can now opt for catheter-based bioprosthetic valve deployment – a procedure that is minimally invasive and eliminates much of the risk associated with previous surgical valve replacement surgeries.
With the introduction of transcutaneous (through the skin) aortic valve replacements, recovery times are greatly reduced. All such valves are made from xenograft biomaterials, and while effective for this application, have limited durability.
Furthermore, the transcutaneous replacement valve designs incorporate thinner, more flexible xenograft biomaterials in order to streamline safer deployment through catheters.
Heart valves are highly complex and function in one of the most mechanically demanding environments in the body. They also remain poorly understood, not surprising given their complex shape and position tucked away inside the heart. So while it stands to reason that developing bioprosthetics that look, feel and function more closely to the native heart valves they replace was a good idea, this new study suggests the introduction of thinner leaflets may produce unintended negative effects.
Computational modeling has enabled accurate visualizations of valve behavior for the first time. And, the study highlights the potentially serious impact of introducing thinner, more flexible tissues into the cardiac system.
Durability is a key factor and the researchers found thinner valve leaflets ‘flutter’ like a flag in order to open and close the valve through millions of cycles that allow for natural blood circulation.
“Valvular designs that are too thin flutter and this compromises their durability and in turn can induce blood cell damage,” said Dr. Thomas J.R. Hughes.
“All these fluttering effects are cumulative, and may limit the bioprosthetic heart valve’s durability,” added Dr. Sacks.
“The ability to look at this phenomenon in-silico (on a computer) for the first time allows us to determine how the leaflets undergo fatigue and assess what’s needed to improve their durability – new design, new materials, or both.”
While the study builds upon decades of research conducted by researchers from the Oden Institute and Iowa State University, it could not have been made possible without access to the supercomputing power made available by the Texas Advanced Computing Center (TACC) at UT Austin. All simulations were generated on TACC’s ‘Stampede’ system.
“It cannot be understated just how important the role of facilities like TACC have played in the ever-improving accuracy of computational engineering and science simulations,” said Dr. Thomas Hughes.
###
Media Contact
John Holden
[email protected]
Original Source
https:/