For some leukemia patients, the only potential chemotherapy option is a drug that also carries a high risk of heart failure. This means that some patients who recover from their cancer will end up dying of heart disease brought on by the cure.
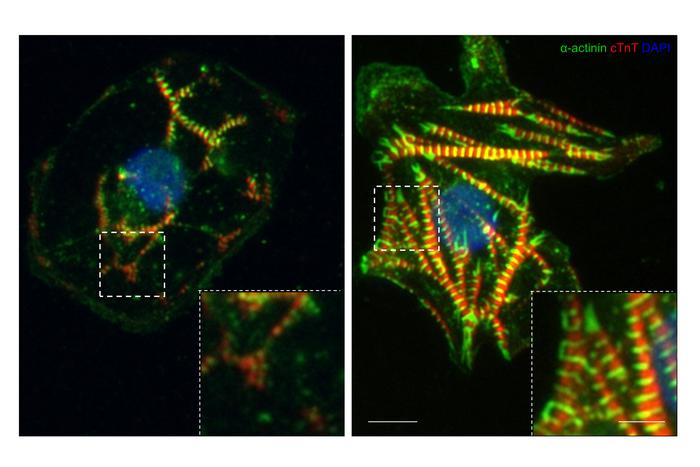
Credit: Image courtesy of the researchers
For some leukemia patients, the only potential chemotherapy option is a drug that also carries a high risk of heart failure. This means that some patients who recover from their cancer will end up dying of heart disease brought on by the cure.
In a new study, researchers from the University of Illinois Chicago and other universities have identified mechanisms that cause the drug, ponatinib, to harm the heart. They also identified a promising treatment that could reverse this process. The paper, with senior author Sang Ging Ong, assistant professor of pharmacology and medicine at UIC, is published in Circulation Research. The study is part of a growing field called cardio-oncology that investigates drugs that shrink tumors but can also cause heart problems.
While there are three options of drugs for treating chronic myeloid leukemia, many patients are resistant to the other two, leaving ponatinib as their only choice.
“These patients have no other options for treatment,” Ong said, despite the concerns about the drug’s side effects. In fact, ponatinib was pulled from the market for a few months after its introduction in 2012 because of concerns about heart problems.
The researchers were interested in understanding the interaction between ponatinib and the heart cells responsible for contraction. They discovered that ponatinib damages these cells by activating a process known as the integrated stress response.
The mechanism for this is related to the functioning of a kinase — an enzyme involved in energy transfer — called GCN2. The researchers found that ponatinib, despite being a kinase inhibitor, actually activates GCN2, which in turn switches on the integrated stress response. While this response isn’t always a bad thing — its purpose is to protect cells — it can also lead to their death under prolonged stress.
To see if this response was harming the cells, the researchers studied what would happen if they used a small molecule to block the integrated stress response in both cells and in mice during ponatinib treatment. They found that the treatment helped protect heart cells from the damaging side effects of the drug yet did not diminish ponatinib’s tumor-fighting efficacy.
“It protects the heart but at the same time, it still allows us to kill cancer cells,” Ong said.
More research is needed to know if this protective measure would work well in humans, Ong said. The mechanisms they identified are important in other cardiac diseases, as well, which could lead to future research on how to protect cells against different conditions.
Ong’s co-senior authors on the study are Won Hee Lee at the University of Arizona and Sang-Bing Ong at the Chinese University of Hong Kong. Other UIC authors at the College of Medicine or University of Illinois Cancer Center are Gege Yan, Zhenbo Han, Youjeong Kwon, Jordan Jousma, Sarath Babu Nukala, Xiaoping Du and Sandra Pinho, as well as Benjamin Prosser from the University of Pennsylvania.
Written by Emily Stone
Journal
Circulation Research
DOI
10.1161/CIRCRESAHA.123.323683
Article Title
Integrated Stress Response Potentiates Ponatinib-Induced Cardiotoxicity
Article Publication Date
7-Feb-2024
COI Statement
none



