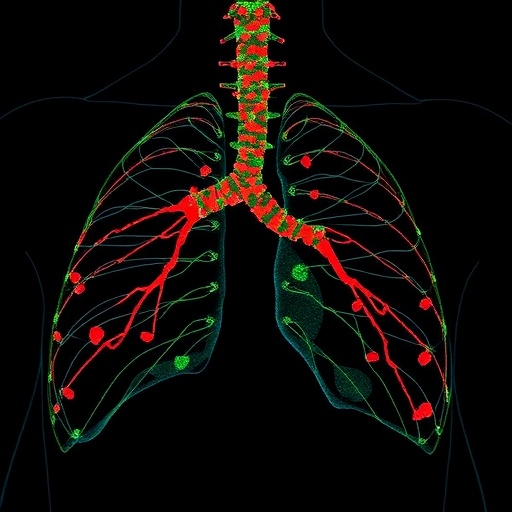
In the relentless search for reliable cancer biomarkers, a groundbreaking study has illuminated the role of circulating Heat Shock Protein 70 (Hsp70) as a pivotal indicator of tumor progression and relapse in thoracic cancers. Thoracic malignancies, notably non-small cell lung cancer (NSCLC), remain among the leading causes of cancer-related mortality worldwide. Their insidious capacity for early metastasis and therapeutic resistance has posed formidable challenges to clinicians and researchers alike. The latest research published in BMC Cancer unveils the intricate relationship between extracellular Hsp70 levels in patient plasma and the aggressiveness of thoracic tumors, marking a potential paradigm shift in how oncological prognostication and treatment monitoring may be approached.
The study concentrated on evaluating circulating extracellular Hsp70 (eHsp70) in the plasma of patients diagnosed with NSCLC, as well as those harboring lung metastases originating from extrathoracic cancers, prior to undergoing surgical intervention. By utilizing a highly sensitive Hsp70-exo ELISA assay, which selectively detects microvesicle-associated forms of eHsp70, the researchers were able to quantify circulating levels and investigate correlations with disease stage and immune profile. Complementing this biochemical approach, detailed immunophenotyping of peripheral blood lymphocytes by flow cytometry shed light on the systemic immune alterations that accompany tumor progression.
.adsslot_1fZD3qCt59{ width:728px !important; height:90px !important; }
@media (max-width:1199px) { .adsslot_1fZD3qCt59{ width:468px !important; height:60px !important; } }
@media (max-width:767px) { .adsslot_1fZD3qCt59{ width:320px !important; height:50px !important; } }
ADVERTISEMENT
Findings revealed a stark elevation in circulating eHsp70 concentrations in NSCLC patients relative to healthy controls, underscoring its potential as a discriminative biomarker. Importantly, no significant difference in eHsp70 levels was observed between the adenocarcinoma and squamous cell carcinoma subtypes, suggesting a pan-NSCLC relevance of this marker. The study also demonstrated a stepwise increase in eHsp70 in parallel with advancing clinical stages culminating in metastatic disease, reflecting an ongoing escalation of tumor burden and aggressiveness.
Among the most salient discoveries was the association of heightened eHsp70 levels with lymph node metastases—a critical prognostic factor in thoracic oncology. Patients with nodal involvement exhibited markedly higher plasma eHsp70, reinforcing the protein’s utility in detecting early metastatic spread that might otherwise evade conventional imaging modalities. This correlation extends the utility of eHsp70 from an indicator of tumor presence to a marker distinguishing more advanced disease states, thus empowering clinicians with actionable insights prior to surgery.
Further entwining tumor biology with host immunity, the research illuminated profound alterations in lymphocyte populations among thoracic cancer patients. There was a consistent reduction in total lymphocyte counts—a hallmark of systemic immune depression often exploited by tumors to evade eradication. An increase in immunoregulatory T cells (Tregs) was also observed, pointing toward a tumor-fostered immunosuppressive milieu that can blunt anti-tumor immune responses and facilitate progression.
Crucially, elevated pre-surgical eHsp70 levels were strongly predictive of early disease relapse following ostensibly curative resection. This insight is transformative, offering a non-invasive biomarker to stratify patients at highest risk for therapeutic failure and recurrence, thereby enabling intensified surveillance or adjunct treatment strategies. Early identification of such patients could streamline precision oncology workflows, curtailing morbidity and improving survival outcomes.
Mechanistically, the source of circulating eHsp70 as membrane-expressed protein-loaded extracellular vesicles posits a functional conduit by which tumor cells influence their microenvironment and immune contexture. These microvesicles might mediate intercellular communication, foster metastatic niche formation, and modulate immune surveillance—pathways ripe for therapeutic targeting. The implications of this dynamic underscore the multifaceted role of Hsp70 beyond a mere biomarker, positioning it at the nexus of oncogenesis and immune evasion.
The robustness of the Hsp70-exo ELISA assay used in this investigation, designed to measure microvesicle-associated Hsp70 specifically, is a technical leap overcoming previous limitations in detecting extracellular chaperones amidst the complex plasma milieu. This methodological advancement ensures reliable quantification correlating tightly with clinical parameters, thus bolstering the translational feasibility of this biomarker in routine oncology practice.
Contextualizing these findings within the broader landscape of thoracic oncology, circulating eHsp70 emerges as a multifaceted marker that encapsulates tumor biology, metastatic potential, and immune dysregulation. Its measurement could complement imaging and histopathological assessments, potentially serving as a cornerstone in individualized patient management algorithms. Moreover, its predictive capability for early relapse positions it as an indispensable tool in post-surgical patient stratification.
While this study primarily focused on NSCLC and thoracic metastases, the ubiquity of Hsp70 overexpression across cancer types beckons further research into its applicability as a universal biomarker. Future investigations may unravel whether interventions targeting Hsp70 expression or its vesicular release can stymie tumor progression or sensitize tumors to existing therapies, heralding novel therapeutic avenues.
In summary, the elucidation of circulating extracellular Hsp70 as a sensitive and specific biomarker heralds a promising frontier in thoracic cancer diagnostics. By bridging tumorigenesis and immune response parameters, it offers a holistic snapshot of disease state and therapeutic outlook. As the oncology community continually leans towards minimally invasive precision medicine, such innovations stand to revolutionize patient care paradigms, improving detection, prognostication, and ultimately, survival in thoracic malignancies.
Subject of Research: Circulating extracellular Heat Shock Protein 70 (eHsp70) as a predictive biomarker for lymph node metastases and early relapse in thoracic cancers, including non-small cell lung cancer and metastases from extrathoracic primary tumors.
Article Title: Circulating Hsp70: a tumor biomarker for lymph node metastases and early relapse in thoracic cancer
Article References:
Lobinger, D., Taylor, N., Messner, V. et al. Circulating Hsp70: a tumor biomarker for lymph node metastases and early relapse in thoracic cancer. BMC Cancer 25, 1297 (2025). https://doi.org/10.1186/s12885-025-14725-5
Image Credits: Scienmag.com
DOI: https://doi.org/10.1186/s12885-025-14725-5
Tags: BMC Cancer study findingscancer metastasis monitoringcirculating Heat Shock Protein 70early thoracic cancer spreadextracellular Hsp70 levelsmembrane-bound Hsp70 functionmicrovesicles in cancer researchnon-small cell lung cancer biomarkersoncological prognostication methodstherapeutic resistance in thoracic malignanciestumor activity measurement techniquestumor progression indicators