In a large retrospective study, investigators identify a significant treatment gap in managing patients with and at risk for clinical atherosclerotic cardiovascular disease, reports the Canadian Journal of Cardiology
Credit: Canadian Journal of Cardiology
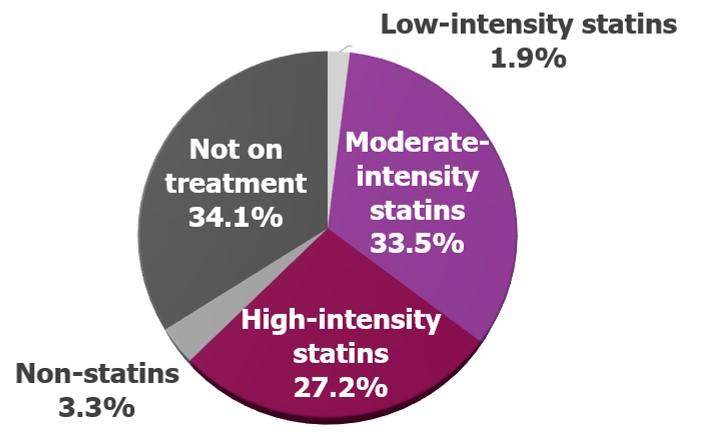
Philadelphia, July 15, 2019 – Statins, the most commonly used effective lipid-lowering drugs, are significantly underutilized to treat lipid abnormalities in patients with and at risk for atherosclerotic cardiovascular disease (ASCVD), according to a retrospective study of more than 280,000 patients in Alberta, Canada. Investigators report in the Canadian Journal of Cardiology, published by Elsevier, that only two-thirds of these patients were receiving moderate/high-intensity statins, and of the ones treated, more than a third are under-treated based on the fact that they did not achieve recommended low-density lipoprotein cholesterol (LDL-C) levels at follow-up testing.
It should be noted that numerous studies have documented the benefits of appropriate statin use in at-risk populations, demonstrating reduction in atherosclerotic disease and the prevention of adverse outcomes like heart attacks, strokes, and deaths.
“Despite the known benefits of statins, a significant treatment gap persists in patients with ASCVD or at high risk of developing ASCVD. We need to conduct additional research to better understand contemporary management of these patients,” said lead investigator Guanmin Chen, PhD, MD, MPH, Medlior Health Outcomes Research Ltd; Department of Community Health Sciences and Libin Cardiovascular Institute of Alberta; and O’Brien Institute for Public Health, Cumming School of Medicine, University of Calgary, Calgary, AB, Canada.
Investigators assessed current patterns of lipid-lowering therapy for the management of LDL-C among 281,665 patients identified with ASCVD, based on administrative health system data for 2011-2015 from the province of Alberta. A retrospective study was conducted by linking multiple health system databases to examine clinical characteristics, treatments, and LDL. The objectives of the study were to characterize the proportion of patients with ASCVD and a statin prescription; to describe the intensity level of statins prescribed; and to determine the proportion of statin users who achieved recommended levels of LDL-C.
LDL-C was assessed at the first measurement (index test) and second measurement (follow-up test) during the study period. LDL-C levels were evaluated based on the 2016 Canadian Cardiovascular Society guideline recommendations for achieving less than 2.0 mmol/L or a 50 percent reduction. Statin therapies were categorized as low-, moderate-, and high-intensity.
Among the individuals identified with ASCVD during the study period, 78 percent had an index LDL-C test and 66 percent were prescribed lipid-lowering therapy. Most patients receiving any lipid-lowering therapy were on moderate-/high-intensity statins. Failure to achieve guideline-recommended levels of LDL-C was common among patients using moderate- or high-intensity statin therapy; and 40 percent of patients did not adhere to their treatment regimens.
“Given the remarkable treatment gap identified in these patients at-risk for ASCVD, the current study results may help to facilitate new strategies to reduce the number of untreated or under-treated patients,” commented Dr. Chen. “Additional research is needed to assess the reasons for the observed treatment gaps and their effects on morbidity, mortality, and other important outcomes, such as health-related quality of life, functional status, as well as healthcare resource utilization and costs.”
The authors recommend several strategies to help reduce this treatment gap: standardizing care through ASCVD-specific admission orders; implementing risk classification tools and corresponding statin treatment recommendations in lab orders; electronic medical record review; and a follow-up lipid profile at the time of discharge. US clinical guidelines have also recently highlighted new lipid-lowering therapies, including PCSK9 inhibitors, as an option for lipid management among very high risk ASCVD patients to lower risk of cardiovascular events.
“This study showed in a large contemporary Canadian population that statins are under-used to lower cholesterol. Increasing uptake of statins could drastically reduce the number of heart attacks, strokes, and death in patients with established vascular disease,” explained co-investigator Todd Anderson, MD, Director, Libin Cardiovascular Institute; Professor & Head, Department of Cardiac Sciences; Professor in the Department of Medicine, Merck Chair, Cardiovascular Research, University of Calgary, Cumming School of Medicine, Calgary, AB, Canada.
In an accompanying editorial, lead author Robert T. Sparrow, MD, Faculty of Medical Science, Schulich School of Medicine and Dentistry, Western University, London, ON, Canada, discusses the challenges of non-compliance, pointing out that statins are often the subject of negative news stories and internet postings that minimize their extremely well-established benefits and exaggerate their adverse effects to a degree not seen with other cardiovascular drugs. Therefore, patient education must often counter pre-existing biases introduced by the media.
“The results of this study bring to light an important principle: time and energy, not knowledge, are the real barriers to statin prescribing. The many health needs and perceptions of ASCVD patients, short appointments, and competing demands on physician time all combine to impede statin prescribing,” commented Dr. Sparrow. “Reminder systems to identify undertreated patients and tools to streamline the treatment discussion process and encourage patient empowerment through education can lead to robust improvements. It is time to lighten the burden on physicians and encourage implementation of systems and programs around them to help improve their prescribing practices.”
Low-density lipoprotein cholesterol (LDL-C) is sometimes called “bad” cholesterol because a high LDL level contributes to a build-up of plaque in the arteries, a condition called atherosclerosis. Measuring LDL-C in the blood is an important indicator in the development and management of ASCVD. The most commonly used medication to treat high LDL-C is a statin, which helps reduce LDL levels by interfering with cholesterol production in the liver.
###
Media Contact
Eileen Leahy
[email protected]
Related Journal Article
http://dx.




