Credit: Sabatino et al, 2020 (PLOS ONE, CC BY 4.0)
COVID-19 patients with cardiovascular comorbidities or risk factors are more likely to develop cardiovascular complications while hospitalized, and more likely to die from COVID-19 infection, according to a new study published August 14, 2020 in the open-access journal PLOS ONE by Jolanda Sabatino of Universita degli Studi Magna Graecia di Catanzaro, Italy, and colleagues.
For most people, the Novel Coronavirus Disease 2019 (COVID-19) causes mild illness, however it can generate severe pneumonia and lead to death in others. It is crucial for clinicians working with cardiovascular patients to understand the clinical presentation and risk factors for COVID-19 infection in this group.
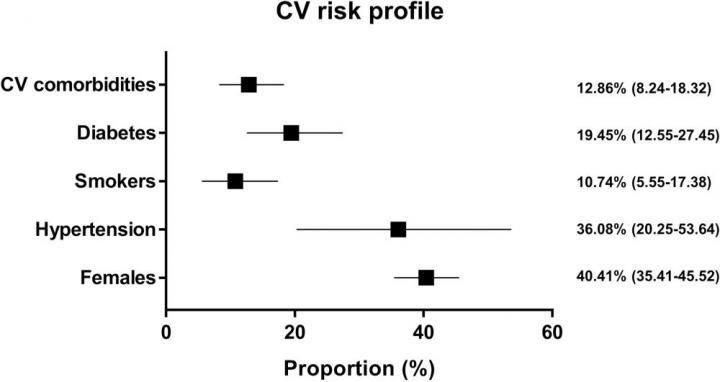
In the new study, researchers analyzed data from 21 published observational studies on a total of 77,317 hospitalized COVID-19 patients in Asia, Europe and the United States. At the time they were admitted to the hospital, 12.89% (95% CI 8.24-18.32) of the patients had cardiovascular comorbidities, 36.08% (95% CI 20.25-53.64) had hypertension and 19.45% (95% CI 12.55-27.45) had diabetes.
Cardiovascular complications were documented during the hospital stay of 14.09% (95% CI 10.26-20.23) of the COVID-19 patients. The most common of these complications were arrhythmias or palpitations; significant numbers of patients also had myocardial injury. When the researchers analyzed the data, they found that pre-existing cardiovascular comorbidities or risk factors were significant predictors of cardiovascular complications (p=0.019), but age (p=0.197) and gender (p=0.173) were not. Both age and pre-existing cardiovascular comorbidities or risk factors were significant predictors of death.
The authors add: “Cardiovascular complications are frequent among COVID-19 patients and might contribute to adverse clinical events and mortality.”
###
Citation: Sabatino J, De Rosa S, Di Salvo G, Indolfi C (2020) Impact of cardiovascular risk profile on COVID-19 outcome. A meta-analysis. PLoS ONE 15(8): e0237131. https:/
Funding: The author(s) received no specific funding for this work.
Competing Interests: The authors have declared that no competing interests exist.
In your coverage please use this URL to provide access to the freely available article in PLOS ONE: https:/
Media Contact
Prof. Salvatore De Rosa
[email protected]
Related Journal Article
http://dx.




