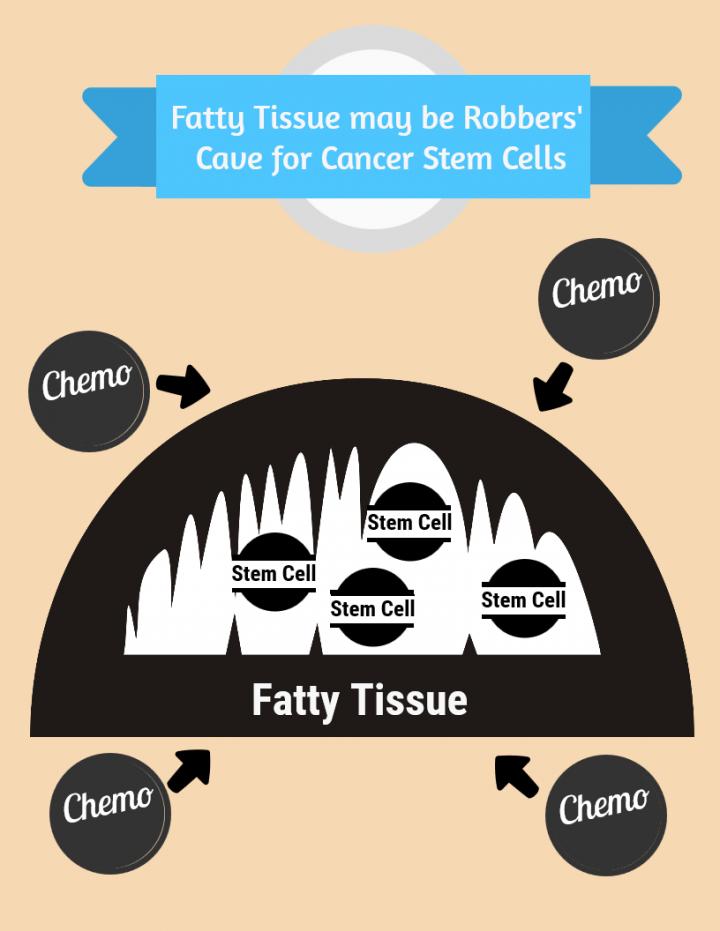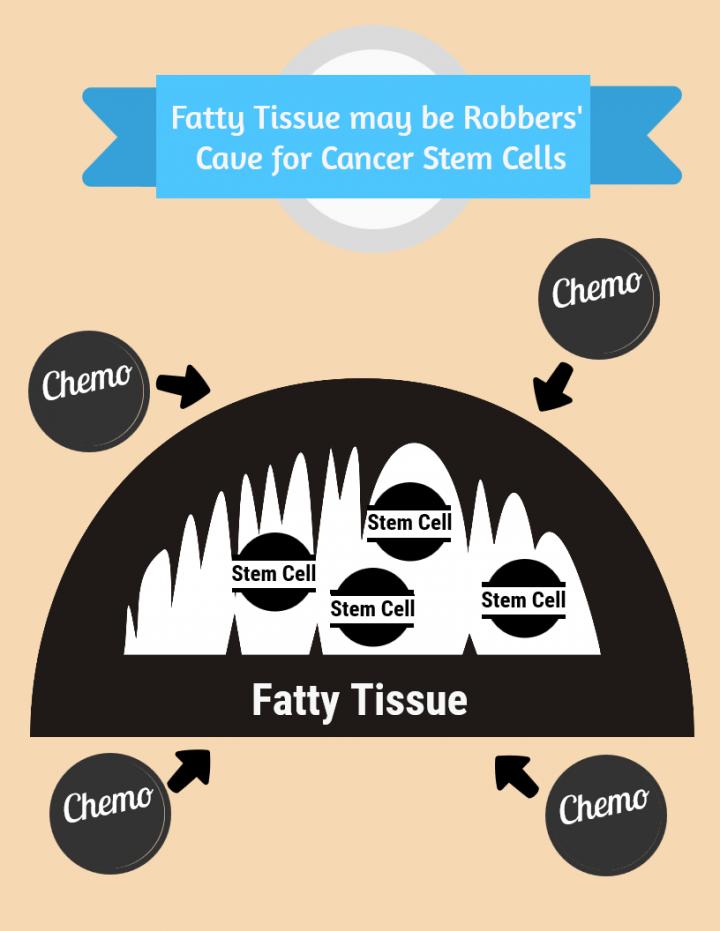
Across many cancer types, obese patients fare worse than leaner patients. Now a University of Colorado Cancer Center study published in the journal Cell Stem Cell offers a compelling hypothesis why: researchers found that leukemia stem cells “hide” in fatty tissue, even transforming this tissue in ways that support their survival when challenged with chemotherapy. It is as if leukemia stem cells not only use fatty tissue as a robbers’ cave to hide from therapy, but actively adapt this cave to their liking.
“It’s been increasingly appreciated that cancer can originate in stem cells and that failing to kill cancer stem cells can lead to relapse. Researchers have also come to appreciate the importance of surrounding tissues — the ‘niche’ or tumor microenvironment — in supporting cancer stem cells. In leukemia, the obvious niche is the bone marrow, but little attention has been paid to other sites in the body. This study is one of the first to evaluate adipose tissue, fat, as a possible tumor-supporting niche,” says Craig Jordan, PhD, investigator at the CU Cancer Center and Nancy Carroll Allen Professor of Hematology in the CU Department of Medicine.
Jordan describes how the “very original and insightful” line of reasoning of first author, Haobin Ye, PhD, was essential for the study. First, obese leukemia patients have poorer outcomes. Second, stem cells drive growth, resist therapy and can create relapse in leukemia. Third, the tumor microenvironment is important to cancer stem cells. At the intersection of obesity, stem cells and tumor microenvironment is adipose tissue — could stem cells in fatty tissue cause poorer prognosis in obese patients?
The group started by examining cancer cells found in the adipose tissue of a mouse model of leukemia. Rather than the expected mix of regular cancer cells with cancer stem cells, the group found that this fatty tissue was enriched for cancer stem cells. No lowly sneak-thieves were these – it was the master thieves of cancer stem cells that exploited the robbers’ cave of fatty tissue. Not only was there a disproportionately high ratio of stem cells in adipose tissue, but these stem cells used a different energy source than stem cells in the bone marrow microenvironment – appropriately, these stem cells in fatty tissue powered their survival and growth with fatty acids, manufacturing energy by the process of fatty acid oxidization. In fact, these adipose tissue stem cells actively signal fat to undergo a process called lipolysis which releases fatty acids into the microenvironment.
“The basic biology was fascinating: the tumor adapted the local environment to suit itself,” Jordan says.
Finally, when the group challenged these cells with chemotherapy they discovered that stem cells in fatty tissue that had switched their energy source to fatty acids were more resistant than stem cells outside this tissue. When Ye, Jordan and colleagues examined samples of human leukemia, they found characteristics similar to the mouse models — cells specialized to use fatty acids as their energy source were more resistant to chemotherapy.
“Perhaps in the context of chemotherapy treatment, these stem cells in adipose tissue might be harder to kill than stem cells in the bone marrow,” Ye says.
If further work bears out this hypothesis, it could help to explain the fact of poorer outcomes in obese patients. The group plans to continue studies with mouse models of varying obesity, potentially shedding light on whether more adipose tissue provides either more energy or a larger robbers’ cave for cancer stem cells evading treatment.
###
Media Contact
Garth Sundem
[email protected]
@CUAnschutz
http://www.ucdenver.edu
The post Cancer stem cells in ‘robbers cave’ may explain poor prognosis for obese patients appeared first on Scienmag.