In a groundbreaking exploration of the complex mechanisms behind multiple myeloma, researchers Jiang, Zhang, and Peng have uncovered an intriguing relationship between complement component C3a and the formation of osteoclasts. This research sheds new light on the biological pathways that govern bone resorption, a critical aspect of multiple myeloma pathology. The findings were recently published in the renowned journal, Journal of Translational Medicine, raising questions about potential therapeutic strategies that could emerge from this new understanding.
Understanding the role of osteoclasts in the context of multiple myeloma is paramount to addressing the complications that arise from this disease. Osteoclasts are specialized cells responsible for bone resorption, a process that, when dysregulated, leads to bone fragility and pain, which are common in patients afflicted by multiple myeloma. The study demonstrates that complement C3a, a peptide involved in the immune response, plays a surprisingly pivotal role in promoting osteoclastogenesis, highlighting the connection between immune signaling and bone metabolism.
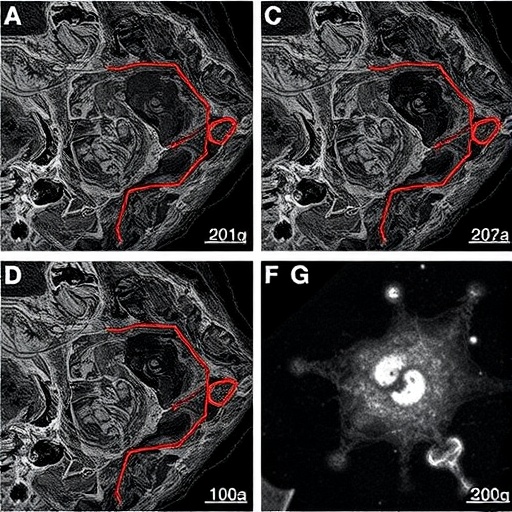
The mechanism proposed by the authors revolves around the inhibition of Sirt1, a protein known to act as a cellular regulator of metabolism and aging. Sirt1 has been recognized for its protective effects on bone density and the inhibition of osteoclast differentiation. The research elucidates a novel pathway whereby C3a’s action leads to diminished Sirt1 levels, thereby facilitating the activation of critical signaling pathways like PI3K, PDK1, and SGK3 that ultimately promote osteoclast formation. This finding bridges the gap between the immune system and bone health, a concept previously overlooked in the context of hematological malignancies.
Delving deeper into the implications of reduced Sirt1 activity, the researchers emphasize that this change may create a permissive environment for osteoclast differentiation. By crippling the protective mechanisms that Sirt1 provides, C3a effectively paves the way for osteoclastogenesis. This means that targeting the C3a pathway could present an innovative therapeutic approach, offering potential avenues for preventing bonerelated complications in multiple myeloma patients.
As these findings gain traction, they open up discussions about the broader implications of complement proteins in bone diseases. Traditionally, the complement system has been primarily associated with the innate immune response, but this study hints at its essential roles in skeletal homeostasis as well. The intricate interplay between immune factors and bone metabolism suggests that treatments aimed at modulating the complement system could yield benefits not only in cancer therapies but also in combating osteoporosis and other bone disorders.
The activation of the PI3K/PDK1/SGK3 pathway by C3a further complicates the picture. These signaling pathways are known for their influence on cell survival, metabolism, and differentiation. Understanding how these cascades interact with osteoclast differentiation will be crucial for devising therapeutic interventions aimed at mitigating bone loss in multiple myeloma and potentially other malignancies. This study should catalyze more research into how immune signaling influences skeletal health, particularly in the context of diseases characterized by altered bone metabolism.
Interestingly, the findings also lead to questions about the timing and context of C3a’s effects. The study suggests a critical role during the progression of multiple myeloma, yet it remains to be determined whether manipulating C3a levels could have protective effects at different stages of disease or in early intervening scenarios. Future clinical studies will be necessary to elucidate whether inhibiting C3a or enhancing Sirt1 can indeed yield favorable outcomes for patients on the brink of advanced stages of multiple myeloma.
As researchers look into potential interventions, a deeper understanding of the molecular interactions can aid in the identification of suitable candidates for clinical trials. By leveraging the molecular insights gained from the current study, researchers may identify new pharmaceutical agents that could inhibit C3a’s activity or enhance Sirt1’s functions, providing a multi-pronged approach to treat or even prevent skeletal complications in myeloma patients.
The publication of these findings is timely, as the medical community is increasingly aware of the need for integrative approaches to cancer care. This research underscores the importance of examining cancer not only as a disease that necessitates aggressive systemic therapies but also as a condition that deeply interacts with the body’s physiological systems, including bone and immune responses. Future studies will undoubtedly seek to integrate this knowledge into comprehensive therapeutic frameworks for myeloma patients.
The potential for these findings to influence guidelines for clinical practice is significant. As oncologists and hematologists investigate the best methods for managing bone health in their patients, understanding how complement proteins impact osteoclast activity may lead to more holistic treatment strategies. Recommendations might soon emphasize collaborative efforts between oncologists and specialists in bone health, particularly in patients suffering from the skeletal complications of multiple myeloma.
In summary, the research led by Jiang, Zhang, and Peng reveals the critical relationship between complement C3a and osteoclastogenesis through Sirt1 inhibition, uncovering novel pathways that may inform future therapeutic strategies for multiple myeloma. The implications extend beyond this specific type of cancer, hinting at broader applications in the understanding of bone metabolism and immune responses. As ongoing research continues to unravel these complex interactions, it is clear that the intersection of immunology and oncology will be a fertile ground for future discoveries.
In conclusion, the study’s findings represent a pivotal step forward in our understanding of how immune mediators influence bone health in patients with multiple myeloma. As this line of inquiry progresses, it promises to reshape how clinicians approach the multifaceted challenges of treating patients with this complex disease. The confluence of immune and skeletal health highlights the need for ongoing research and collaborative efforts to enhance patient outcomes in hematological malignancies.
Subject of Research: The role of complement C3a in osteoclast formation and bone health in multiple myeloma patients.
Article Title: Correction: Complement C3a promotes the formation of osteoclasts by inhibiting Sirt1 to activate the PI3K/PDK1/SGK3 pathway in patients with multiple myeloma.
Article References:
Jiang, F., Zhang, Y., Peng, F. et al. Correction: Complement C3a promotes the formation of osteoclasts by inhibiting Sirt1 to activate the PI3K/PDK1/SGK3 pathway in patients with multiple myeloma.
J Transl Med 23, 1329 (2025). https://doi.org/10.1186/s12967-025-07335-z
Image Credits: AI Generated
DOI: 10.1186/s12967-025-07335-z
Keywords: multiple myeloma, osteoclasts, complement C3a, Sirt1, PI3K pathway, bone health, immunology, signaling pathways.
Tags: bone fragility in myeloma patientsbone resorption mechanismsC3a complement proteincomplement system in cancerimmune signaling and bone metabolismimplications for myeloma treatment.multiple myeloma pathologyosteoclast formation in myelomaosteoclastogenesis and bone healthSirt1 protein regulationtherapeutic strategies for myelomatranslational medicine research.