Inhibiting the enzyme SCD and blocking the function of the transcription factor FOSB, blunts acquired resistance and extends survival in mouse models of glioblastoma; these findings may also apply to others cancers such as melanoma, say experts
Credit: Cincinnati Children’s
In far too many cases over the years, scientists have discovered promising new cancer treatments, only to report later that the tumor cells found ways to become resistant. These disappointing results have made overcoming drug resistance a major goal in cancer research.
Now, experts at Cincinnati Children’s report success at averting drug resistance in a subtype of brain tumors called glioblastomas. Importantly, the research indicates that the approach may also work in other cancers, such as melanoma, that exhibit a similar pathway of drug resistance.
The method involves inhibiting a protein called SCD and reducing the expression of the transcription factor FOSB (which regulates SCD), so that the tumor cells cannot acquire resistance to the SCD inhibitor. Results were published online Feb. 10, 2021, in the journal Science Advances.
“This is one of the most significant findings from our lab in recent years,” says principal investigator Biplab Dasgupta, PhD, Division of Oncology.
Much more research is needed before this approach can be tested in people with glioblastomas, but animal model experiments reveal that mice bearing brain tumors survive longer when treated with a combination therapy that includes SCD and FOSB inhibition.
Additionally, using the standard of care chemotherapeutic agent temozolomide (TMZ), mice with advanced tumors initially showed “significant” tumor reduction, but all of the mice relapsed and 80% had died by 50 days post treatment. In contrast, when treated with TMZ in combination with the SCD inhibitor, 80% of the mice survived past 50 days.
How the combination therapy works
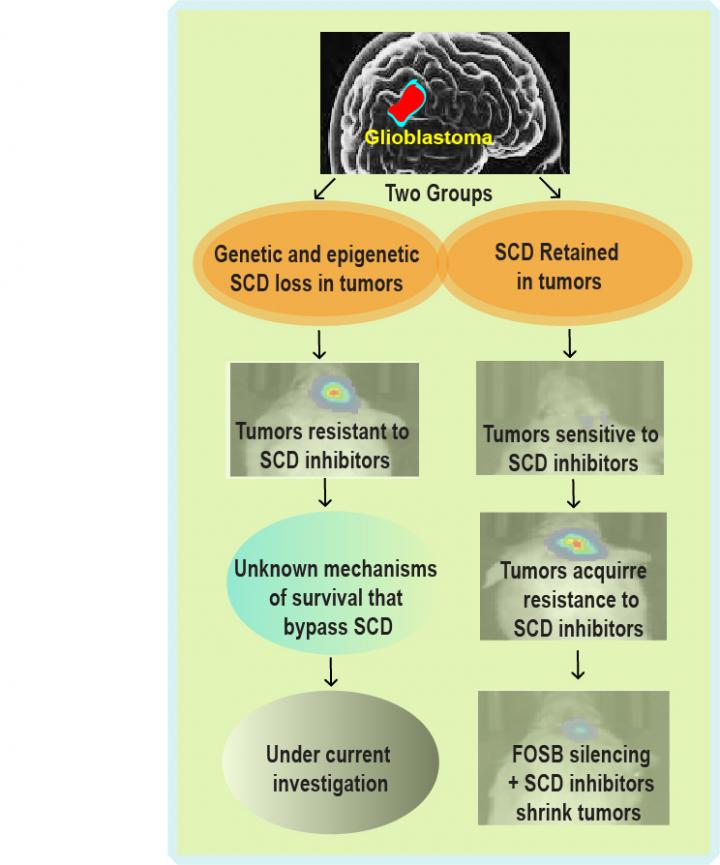
The new approach was based on their discovery that some brain tumors have surprisingly low amounts of an enzyme called Stearoyl Co-A Desaturase (SCD). Typically, cancer cells use elevated levels of this enzyme to fuel their uncontrolled growth, which has inspired a number of drugs that target SCD to treat tumors.
However, through analysis of publicly available glioblastoma genetic datasets, Dasgupta and research fellow Nicole Oatman, PhD, discovered that the SCD gene is both deleted as well as its expression suppressed through epigenetic mechanisms in a large subset of glioblastoma patients.
“This finding was surprising given the requirement of SCD in most cancers,” says Dasgupta.
While the Dasgupta Lab is still working to understand how glioblastomas survive without SCD, potentially by using alternative pathways that bypass SCD, they determined that glioblastoma cell lines that retain SCD are exquisitely sensitive to SCD inhibitors.
They also found that like most cancer cells, SCD inhibitor-sensitive glioblastomas ultimately acquire resistance to SCD inhibitors. They discovered that FOSB protein plays a central role in regulating SCD levels. When a drug knocks down SCD, FOSB kicks in to rapidly build SCD levels back up. This reinforcing effect overwhelms the anti-SCD medication effects and allows tumors to come roaring back.
Turning off the FOSB protein essentially silences the call for reinforcements, which allows the SCD-inhibiting drugs to be dramatically more effective. The team then expanded their work by finding similar outcomes when testing the combination therapy to treat melanoma, a severe form of skin cancer.
By understanding how this process works, Dasgupta says it will help many scientists re-assess clinical trial results for SCD-inhibiting drugs, which may reveal that some past discoveries that appeared to be failures might still have value in cancer treatment.
###
About this study
In addition to Dasgupta and Oatman, co-authors included researchers from Cincinnati Children’s Divisions of Human Genetics, Experimental Hematology and Cancer Biology, Biomedical Informatics, Developmental Biology, and the Center for Autoimmune Genomics and Etiology.
Contributors also included researchers with the University of Cincinnati, Brigham and Women’s Hospital, Boston; the University of California, San Diego; Memorial Sloan Kettering Cancer Center, NY; and the University of Colorado campus in Aurora, CO.
This work was supported by multiple National Institutes of Health grants (ES007250, NS044080, R01NS097266, R01NS075291 and R01NS099161); Endowed Scholar, Pilot Innovation, and CpG grant awards from Cincinnati Children’s; and Cancer Center Affinity and Brain Tumor Center grant awards from the University of Cincinnati.
Media Contact
Tim Bonfield
[email protected]
Related Journal Article
http://dx.




