A groundbreaking meta-analysis published in the flagship oncology journal Oncotarget on May 9, 2025, unveils a critical link between the ABO blood group system and breast cancer susceptibility. This comprehensive investigation spearheaded by researchers Rahaf Alchazal of Yarmouk University and Khaled J. Zaitoun from Johns Hopkins University School of Medicine alongside Jordan University of Science and Technology systematically reviews and synthesizes data from 29 separate studies, cumulatively involving over 13,000 breast cancer patients and a vast control population exceeding 717,000 individuals. The scale and methodological rigor of this study provide unprecedented clarity on the previously ambiguous association between blood group antigens and breast malignancy risk.
Breast cancer remains the most diagnosed cancer among women globally, necessitating ongoing identification of risk factors that contribute to its pathogenesis. While lifestyle and genetic predispositions have been extensively studied, this meta-analysis shifts focus to the biological interface of blood group antigens—proteins and glycoproteins expressed on the surface of erythrocytes and various tissues. The ABO system comprises four primary phenotypes: A, B, AB, and O, differentiated by the presence or absence of A and B antigenic determinants. The Rh factor, a separate, crucial antigen primarily significant in transfusion medicine, was concurrently evaluated for its correlation with breast cancer risk.
Across multinational cohorts spanning Asia, Europe, Africa, and the Americas, the investigators uncovered a distinctive pattern: individuals bearing blood group A demonstrate an 18 percent increased risk of developing breast cancer compared to those with blood group O. This statistically robust association suggests that the presence of A antigens may modulate oncogenic processes within breast tissue, potentially through immune modulation or altered cellular adhesion and signaling pathways. Intriguingly, blood groups B and AB, as well as Rh positive or negative status, did not exhibit significant associations, underscoring the specificity of the A antigen’s potential role in breast tumorigenesis.
Mechanistically, the ABO blood group antigens serve functions beyond erythrocyte typing, with expression reported on epithelial and endothelial cells, including those in breast tissue. These carbohydrate epitopes participate in cellular recognition, signal transduction, and intercellular adhesion — processes integral to tissue homeostasis and malignancy initiation. Alterations or overexpression of these antigens could influence the tumor microenvironment, affecting interactions with the immune system and facilitating evasion of immunosurveillance. The altered glycosylation patterns may also impact cell proliferation, migration, and metastatic potential by modulating adhesion molecules and matrix interactions.
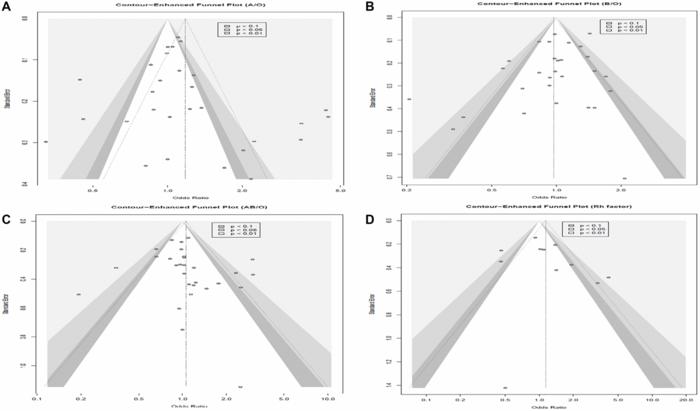
The meta-analytical approach employed by Alchazal and colleagues involves meticulous literature curation from bilateral and multinational databases such as PubMed, Scopus, Web of Science, and Google Scholar. By applying stringent inclusion criteria and advanced statistical modeling to control for heterogeneity and publication bias, the study achieves a refined estimation of risk that surpasses the limitations of individual studies. Funnel plot analyses and sensitivity tests further substantiate the reliability of the findings, reflecting both the study’s methodological robustness and the reproducibility of the observed associations.
Despite these compelling results, the authors caution against interpreting correlation as causation. The complexity of breast cancer etiology encompasses multifactorial genetic, environmental, hormonal, and immunological factors that interplay in intricate pathways. Genetic polymorphisms linked to ABO antigens may be in linkage disequilibrium with oncogenes or tumor suppressor loci, potentially confounding the observed associations. Additionally, population-specific genetic backgrounds and environmental exposures may influence the generalizability of the findings, necessitating validation in diverse cohorts and prospective studies.
The emergent hypothesis that blood type A may serve as a biomarker for breast cancer risk elevates new possibilities in precision medicine. Screening guidelines could be refined to incorporate blood group information, allowing for stratified risk assessments and tailored surveillance regimens. Such approaches align with the growing emphasis on personalized oncology, where genetic and phenotypic markers inform preventative and therapeutic decisions. Moreover, investigating the biochemical and immunological pathways linking blood group antigens to carcinogenesis may identify novel molecular targets for intervention.
Future inquiry must focus on unraveling the molecular underpinnings of this association. Functional studies exploring how the A antigen modifies cellular behavior in breast epithelial cells, impacts immune evasion tactics, and interacts with hormonal signaling pathways are paramount. Expanding research into genome-wide association studies (GWAS) and proteomics analyses could elucidate contributory genetic variants and post-translational modifications underpinning this risk. Parallel examination of the tumor immune microenvironment in relation to ABO blood types might reveal insights into differential immune responses affecting tumor progression.
The significance of this meta-analysis lies not only in its epidemiological insights but also in its potential to catalyze paradigm shifts in cancer prevention and management. It exemplifies the integration of hematologic phenotyping with oncologic risk modeling, a nexus hitherto underexplored in clinical oncology. While further research is imperative to translate these findings into clinical practice, the elucidation of blood group A as a risk factor propels a promising frontier in cancer biology, with far-reaching implications for public health strategies and personalized healthcare.
As researchers worldwide delve deeper into the biological nuances of blood group antigens, this study sets a foundational benchmark and encourages interdisciplinary collaborations bridging hematology, immunology, molecular biology, and epidemiology. The eventual goal is to convert epidemiologic correlations into mechanistic understandings that directly improve patient outcomes through innovative diagnostics and therapeutics.
The dialogue between cancer researchers, clinicians, and molecular biologists ignited by this meta-analysis heralds a new chapter in breast cancer research. If corroborated by future investigations, blood group typing might become a routine element of breast cancer risk profiling, guiding earlier detection efforts that save lives. This promising avenue underscores the transformative potential of leveraging seemingly routine hematological markers to unravel complex disease mechanisms and enhance precision oncology worldwide.
Subject of Research: Not applicable
Article Title: Relationship between ABO blood group antigens and Rh factor with breast cancer: A systematic review and meta-analysis
News Publication Date: May 9, 2025
Web References:
Oncotarget Volume 16 – https://www.oncotarget.com/archive/v16/
DOI: http://dx.doi.org/10.18632/oncotarget.28718
Image Credits: Copyright © 2025 Alchazal et al. This is an open access article distributed under the Creative Commons Attribution License (CC BY 4.0).
Keywords: cancer, breast cancer, cancer risk factors, blood group antigens, tumor
Tags: ABO blood group system and breast cancerAntigenic determinants and malignancyBlood group antigens and healthBlood type A cancer riskBreast cancer research findings 2025Breast cancer susceptibility factorsErythrocyte surface proteins and cancer riskGenetic predispositions to breast cancerImportance of blood type in diseaseLifestyle factors in breast cancerMeta-analysis on breast cancerOncotarget oncology study