Scientists developed a decision support system that relies on expert opinion to prevent anemia in patients with kidney disease
Credit: 2021 Okayama University
Anemia, a condition characterized by the lack of healthy red blood cells in the body, is common in patients with chronic kidney disease who need to undergo routine hemodialysis (a process that helps to “clean” the blood when the kidneys don’t function well). Thus, red blood cell-stimulating agents (called “erythropoiesis-stimulating agents” or ESAs) and iron supplements (ISs) are administered as part of this process. But, complications can arise if the patients have an altered iron metabolism or poor response to medications. Moreover, the medications tend to be expensive and impose a heavy financial burden on public health. Thus, with such patients currently on the rise but not enough physicians suitably trained to administer treatment, additional support systems with smart decision-making capabilities are highly sought after. One option is to turn to artificial intelligence (AI), which seems promising but demands a large dataset and is not practical owing to diverse health conditions of patients.
So, can something be done to improve the situation? In a recent study published in the International Journal of Medical Sciences, medical researchers from Japan tried to find the answer. They came up with a new approach: instead of making the AI learn from the complex physiology of the patient’s body, they opt for a prediction model based on the decisions of experienced physicians. Assistant Professor Toshiaki Ohara from Okayama University, Japan, the lead scientist on the study, explains, “We got the idea while contemplating the thought process of seasoned physicians. After all, they do not calculate detailed values of vital reactions in a patient’s body when deciding dosages, which means prediction models based on biochemistry are not necessary.”
The researchers started off by collecting clinical data at two hospitals in Japan and then preparing two datasets for each hospital: one for training their model and the other for testing and validating its predictions. Simultaneously, they recorded the dosage directions of physicians at both hospitals and considered responses for the two medications used during hemodialysis: ESAs and ISs.
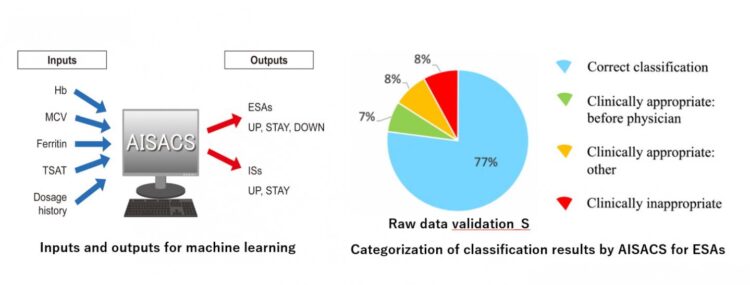
Based on these, they constructed an AI-based model called an “artificial-intelligence-supported anemia control system” (AISACS), which received a total of five inputs (four items of blood examination and dosage history) and churned out dosage direction probabilities for the two medications as outputs. In addition, to make the training process more efficient, they compensated for the time lag between blood examination and dosage decisions by using “data rectification” to match the decision dates with the examination dates.
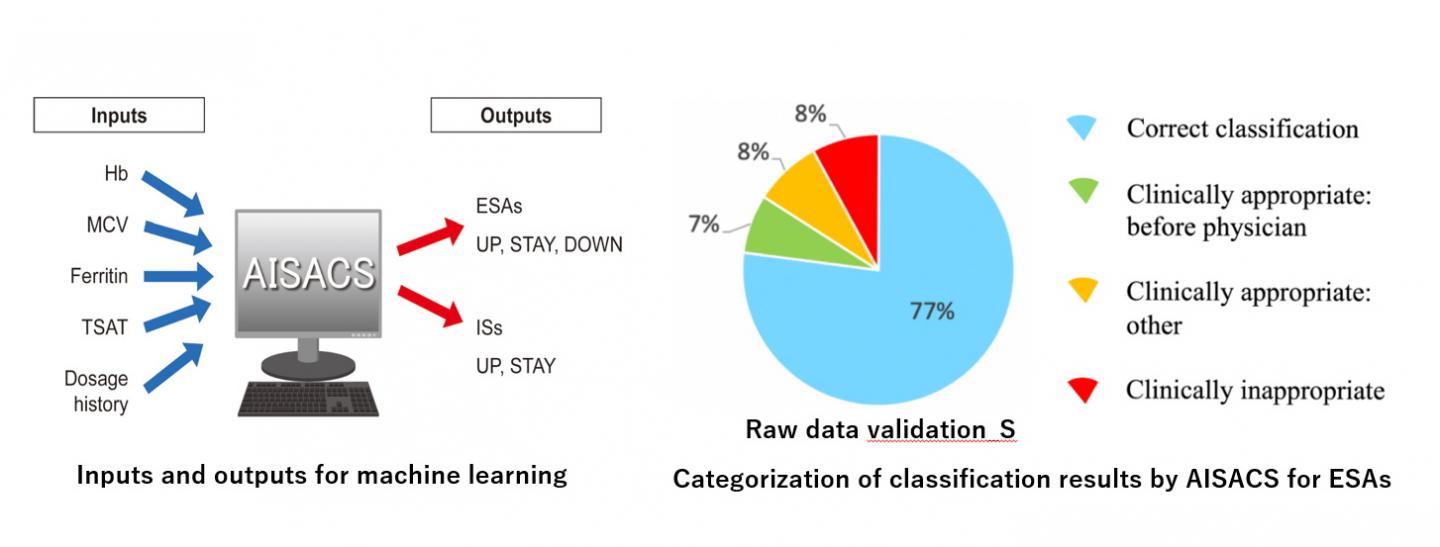
To the researchers’ delight, AISACS showed a high prediction accuracy with correct classification (directions matching those of physicians) rates of 72%-87%. But what was even more interesting was that it provided “clinically appropriate” classifications at even higher rates (92%-97%). These were directions that didn’t match those of physicians (and were sometimes provided ahead of them) but were still considered appropriate from a medical viewpoint.
With these results, researchers are hopeful about AISAC’s future prospects. “By preventing anemia, our system can help alleviate the burdens on physicians and medical insurance systems. Moreover, it has the potential to share the knowledge and experiences related to medications,” comments an excited Dr. Ohara.
Hopefully, this new AI-based approach provides some hope to both patients undergoing hemodialysis and physicians treating them.
###
Media Contact
Toshiaki Ohara
[email protected]
Related Journal Article
http://dx.