In a groundbreaking advancement that could reshape the future of hepatocellular carcinoma (HCC) treatment, scientists have developed an innovative deep learning model capable of accurately predicting microvascular invasion (MVI) using gadoxetic acid-enhanced magnetic resonance imaging (MRI). MVI, a critical prognostic factor, profoundly influences treatment strategies and postoperative outcomes in HCC patients. However, its detection traditionally relies on histopathological examination after surgery, leaving a significant clinical gap for noninvasive, preoperative prediction. Addressing this challenge, researchers from multiple esteemed institutions have employed state-of-the-art deep multi-instance learning techniques, marking a pivotal step toward precision oncology.
This multicenter, retrospective study compiled data from 206 HCC patients with pathologically confirmed diagnoses, sourced from three distinct hospitals, ensuring a diverse and robust dataset for model training and validation. The investigative team focused sharply on the hepatobiliary phase images (HBP) of gadoxetic acid-enhanced MRI, a specialized imaging sequence known for its superior liver lesion characterization. To harness the full potential of this imaging modality, three variations of deep learning architectures were meticulously developed and assessed: two-dimensional (2D), three-dimensional (3D), and a novel 2.5-dimensional (2.5D) deep multi-instance learning (MIL) model.
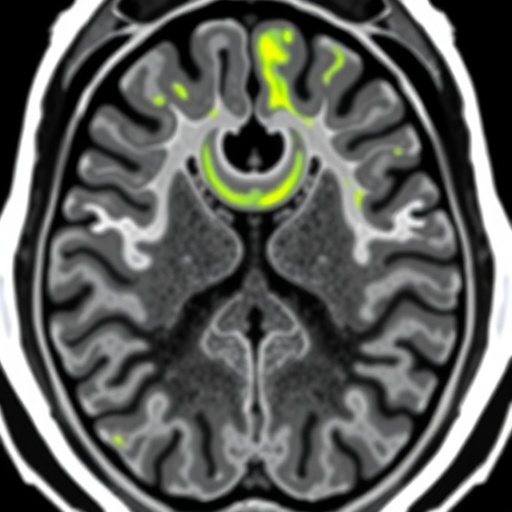
Among these approaches, the 2.5D MIL technique emerged as the most potent, ingeniously integrating information from all axial slices encompassing the tumor and surrounding peritumoral regions. This comprehensive slice selection allowed the model to capture both intratumoral heterogeneity and critical peritumoral microenvironmental features, which are hypothesized to play pivotal roles in MVI development. Remarkably, this approach outperformed conventional models with area under the curve (AUC) values reaching 0.802 in internal validation and 0.759 in the external test cohort, highlighting its strong generalizability across patient populations.
Building on these promising findings, the researchers extended their methodology by incorporating additional MRI sequences—T1-weighted fat-suppressed (T1WI-FS) and T2-weighted fat-suppressed (T2WI-FS) images—into a multimodal prediction framework. The synergistic use of these complementary sequences aimed to further refine the predictive algorithm by capturing distinct tissue contrasts and pathological signatures of MVI. This multimodal deep learning model demonstrated exceptional predictive capacity, with AUC values soaring as high as 0.954 in the training set, and sustaining robust performance metrics with AUCs of 0.857 and 0.788 in independent validation and test sets respectively.
These advancements are not merely incremental; they represent a paradigm shift in medical imaging diagnostics for liver cancer. The exploitation of 2.5D MIL in this context signifies a novel computational strategy that leverages the spatial and contextual richness of MRI datasets more effectively than traditional machine learning or purely 2D/3D frameworks. By embracing the heterogeneous nature of tumor microenvironments across consecutive axial slices, this approach unlocks a more nuanced understanding of tumor biology, which is crucial for preoperative risk stratification.
Importantly, the ability to noninvasively predict MVI preoperatively holds profound clinical implications. Surgeons and oncologists can now potentially tailor treatment regimens with increased precision—deciding between surgical resection, transplantation, or adjuvant therapies based on individualized risk profiles. Moreover, early detection of MVI propensity may guide surveillance intensity post-operation, improving patient outcomes through timely interventions.
The retrospective design of this study, coupled with its multicenter data acquisition, lends credibility to the model’s robustness and applicability across different clinical settings. However, the authors underscore the necessity for prospective trials to validate and eventually integrate these computational tools into routine clinical workflows. Additionally, further research into integrating radiogenomics could uncover deeper mechanistic links between image features and genetic underpinnings of microvascular invasion.
On the technical front, the study exemplifies an exemplary application of advanced artificial intelligence methodologies in oncological imaging. The use of deep learning architectures capable of handling multi-instance learning tasks shows how algorithmic innovation can extract actionable insights from complex and high-dimensional medical images. Fine-tuning such models with diverse MRI sequences reinforces the importance of multimodality in capturing the multifaceted nature of cancer pathology.
This research also emphasizes the crucial role of peritumoral tissue analysis, an often-overlooked area in conventional imaging assessments. The findings suggest that changes in the tumor microenvironment surrounding hepatocellular carcinoma lesions carry significant predictive information, urging the clinical community to expand diagnostic focus beyond tumor margins. Such insights will likely spur new investigations into tumor-stroma interactions and their implications in cancer progression.
Future directions proposed by the research team involve the development of automated MRI preprocessing pipelines and user-friendly software interfaces to democratize the use of their predictive models in community hospitals and cancer centers worldwide. Integrating these outputs with electronic health records and decision-support systems could democratize access to personalized oncology care, aligning with global efforts toward precision medicine.
In conclusion, the creation and validation of a deep multi-instance learning model based on gadoxetic acid-enhanced MRI heralds a new age in the preoperative management of hepatocellular carcinoma. By harnessing the power of 2.5D imaging data and multimodal sequences, this approach offers an unprecedented window into tumor invasiveness, enabling clinicians to make better-informed decisions and ultimately improving patient prognoses. As artificial intelligence continues to evolve, such innovations underscore the transformative potential of combining computational prowess with clinical expertise in battling complex diseases like HCC.
Subject of Research: Microvascular invasion prediction in hepatocellular carcinoma using advanced deep learning models applied to gadoxetic acid-enhanced MRI.
Article Title: Deep multi-instance learning model based on gadoxetic acid-enhanced MRI for predicting microvascular invasion of hepatocellular carcinoma: a multicenter, retrospective study.
Article References: Luo, Y., Zhang, G., Zhong, S. et al. Deep multi-instance learning model based on gadoxetic acid-enhanced MRI for predicting microvascular invasion of hepatocellular carcinoma: a multicenter, retrospective study. BMC Cancer 25, 1626 (2025). https://doi.org/10.1186/s12885-025-14971-7
Image Credits: Scienmag.com
DOI: https://doi.org/10.1186/s12885-025-14971-7
Tags: 2.5D deep learning modelsAI liver cancer predictionDeep Learning in Oncologygadoxetic acid MRIhepatocellular carcinoma treatmenthistopathological examination alternativesmicrovascular invasion detectionMRI imaging techniquesmulticenter medical researchnoninvasive cancer diagnosticspatient outcome prediction in HCCPrecision Medicine Advancements