In the evolving landscape of cancer diagnostics, the accurate identification of lymph node recurrence in postoperative papillary thyroid cancer (PTC) remains a formidable challenge. A groundbreaking study published in BMC Cancer introduces advanced machine learning models combined with radiomic analysis, offering promising avenues to address this diagnostic dilemma with unprecedented precision. The research, stemming from an extensive analysis of CT imaging data, marks a significant stride toward enhancing postoperative management in PTC patients.
Papillary thyroid cancer is among the most common types of thyroid malignancy, often necessitating surgical interventions such as total thyroidectomy. Postoperatively, many patients present with enlarged cervical lymph nodes, a condition that may arise not only from cancerous recurrence but also from benign causes such as inflammation or hyperplasia. This ambiguity complicates clinical decisions and delays timely therapeutic interventions. Recognizing this clinical challenge, the new study leverages the burgeoning field of radiomics, which extracts high-dimensional data from medical images, to refine diagnostic accuracy.
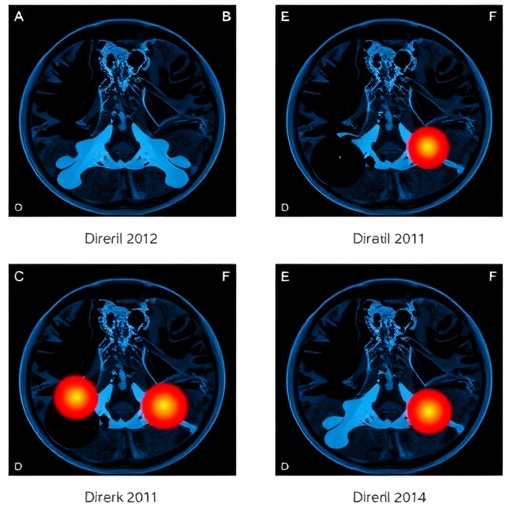
The research undertook a comprehensive retrospective analysis of 194 PTC patients who underwent total thyroidectomy. Out of these, 98 patients exhibited cervical lymph node recurrence, whereas 96 did not. From their enhanced venous phase computed tomography (CT) scans, clinicians meticulously delineated Regions of Interest (ROIs) using 3D Slicer software. A total of 693 lymph nodes were analyzed, including 302 positive (recurrence) and 391 negative (non-recurrence) nodes. The lymph nodes were randomly allocated into training and validation cohorts at a 3:2 ratio, ensuring robust model development and testing protocols.
.adsslot_WNDciy8U9Z{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_WNDciy8U9Z{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_WNDciy8U9Z{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
Radiomics, as employed in this study, involves the quantitative extraction of imaging features that are often imperceptible to the human eye. Using Python-based computational tools, the researchers extracted a vast array of features encompassing texture, shape, intensity, and wavelet-transformed parameters from the delineated ROIs. Through rigorous feature reduction algorithms designed to minimize overfitting and maximize clinical relevance, 35 significant radiomic features emerged as pivotal discriminators between recurrent and non-recurrent lymph nodes.
To translate these radiomic insights into practical diagnostic tools, three distinguished machine learning algorithms were deployed: Lasso regression, Support Vector Machine (SVM), and Random Forest (RF). Each model incorporated the selected radiomic features to predict lymph node recurrence, offering distinct computational advantages. Lasso regression, with its inherent feature selection ability, suited datasets with numerous predictors. The SVM algorithm excelled in handling high-dimensional data and non-linear boundaries, while RF leveraged ensemble decision trees to enhance prediction stability.
Beyond radiomic data, the study integrated clinical risk factors identified through univariate and multivariate analyses. These included patient demographics, tumor staging, and biochemical markers, which were statistically associated with lymph node recurrence risk. By fusing radiomic scores with these clinical parameters, the researchers developed a nomogram—a graphical predictive model—that offers personalized recurrence risk assessment in postoperative PTC patients, paving the way for individualized patient management strategies.
Diagnostic efficacy was robustly evaluated using Receiver Operating Characteristic (ROC) curves, calibration plots, and Decision Curve Analysis (DCA). The ROC analysis demonstrated high area under the curve (AUC) values across all three models, highlighting their superior sensitivity and specificity. Calibration curves confirmed the nomogram’s accuracy in predicting observed outcomes, while DCA revealed its clinical utility by quantifying net benefit across various threshold probabilities for recurrence, supporting decision-making in diverse clinical contexts.
The implications of this study are substantial. Reliable preemptive identification of lymph node recurrence can drastically improve patient outcomes by enabling timely and targeted therapeutic interventions. Moreover, leveraging non-invasive CT imaging enhances patient comfort and safety compared to more invasive biopsy procedures. The integration of machine learning and radiomics heralds a new paradigm in oncologic imaging, where vast, complex data can be harnessed for actionable clinical insights.
While previous imaging studies have primarily relied on morphological criteria, this research underscores the enhanced discriminatory power afforded by radiomics-driven analysis. Such data-driven models mitigate subjective interpretation variability and potentially reduce diagnostic errors. In a clinical environment increasingly focused on precision medicine, these findings offer a scalable and reproducible approach suitable for integration into routine radiologic workflows.
Nonetheless, the study acknowledges inherent limitations, such as its retrospective design and single-center data source, which may influence model generalizability. Future directions include prospective validation across multi-institutional datasets to affirm performance consistency. Additionally, integration with other imaging modalities and molecular biomarkers may further refine predictive accuracy and foster comprehensive diagnostic platforms.
This study is emblematic of the rapid advances in artificial intelligence applications within healthcare. It not only exemplifies how computational methods can unearth hidden diagnostic patterns but also demonstrates the crucial intersection of data science with clinical oncology. As such, these machine learning models hold promise not only for PTC but could be adapted for recurrence diagnostics in other malignancies presenting similar clinical challenges.
In conclusion, the convergence of radiomic analysis and sophisticated machine learning models heralds a transformative leap in postoperative cancer surveillance. This study sets a precedent for leveraging routine CT imaging beyond conventional assessments, unlocking latent data to support clinicians in making informed, precise diagnoses about lymph node recurrence. As research progresses, such innovations are poised to become integral components of cancer management paradigms, ultimately enhancing patient survival and quality of life.
Subject of Research: Postoperative diagnosis of cervical lymph node recurrence in papillary thyroid cancer patients using machine learning and radiomic analysis.
Article Title: Machine learning models for diagnosing lymph node recurrence in postoperative PTC patients: a radiomic analysis
Article References:
Pang, F., Wu, L., Qiu, J. et al. Machine learning models for diagnosing lymph node recurrence in postoperative PTC patients: a radiomic analysis. BMC Cancer 25, 1308 (2025). https://doi.org/10.1186/s12885-025-14594-y
Image Credits: Scienmag.com
DOI: https://doi.org/10.1186/s12885-025-14594-y
Tags: advanced diagnostic techniques for cancerAI in cancer diagnosiscervical lymph node evaluationchallenges in thyroid cancer recurrenceCT imaging in cancer diagnosisenhancing cancer diagnostic accuracy.lymph node recurrence in thyroid cancermachine learning in radiomicspapillary thyroid cancer managementpostoperative thyroid cancer assessmentprecision medicine in oncologyretrospective analysis of thyroid cancer patients