A groundbreaking new study published in the prestigious journal Heart reveals that an artificial intelligence (AI) algorithm, trained solely on routine mammogram images combined with a woman’s age, can predict the risk of major cardiovascular disease with accuracy comparable to the best clinical risk assessment tools currently in use. This innovative approach leverages existing healthcare infrastructure, offering an unexpected yet cost-efficient opportunity for dual-purpose screening that could revolutionize cardiovascular risk detection in women.
Cardiovascular disease (CVD) stands as a leading cause of death worldwide, yet its risk factors tend to be under-recognized and poorly managed among women. Traditional cardiovascular risk prediction models often underperform in females, primarily due to biological differences and gaps in representation during their development. Moreover, modern risk calculators, though improved, generally rely on extensive clinical data, including detailed medical histories and lab results, which are not always available or accessible. This leaves a critical need for simpler, equally reliable predictive tools.
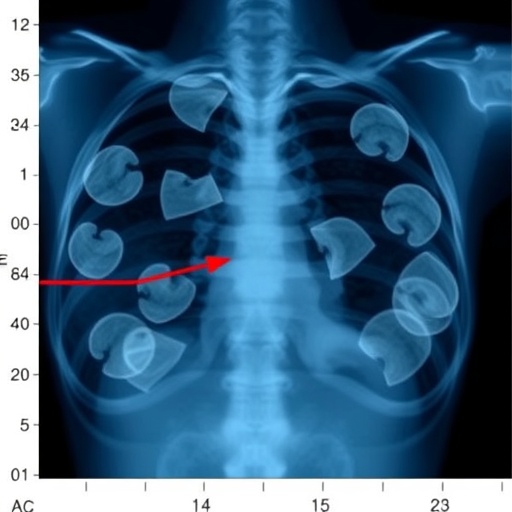
The link between breast arterial calcification (BAC)—a visible marker on mammograms—and CVD risk has intrigued researchers for years. However, BAC alone has proven an inconsistent predictor, partly because it is independent of some common risk factors such as obesity and even negatively correlated with smoking, limiting its standalone utility. Seeking a more comprehensive understanding, researchers hypothesized that analyzing the broader internal composition and tissue characteristics within mammograms might yield a richer, more nuanced source of cardiovascular risk information.
To test this hypothesis, the team analyzed data from 49,196 women enrolled in the Lifepool cohort registry in Victoria, Australia, between 2009 and 2020. The cohort had an average age of 59 and was followed for nearly nine years on average. These women provided essential health background data, including age, smoking status, alcohol intake, body mass index (BMI), diabetes history, and medication use for high blood pressure, cholesterol, and blood thinning. Additional contextual factors such as menopause status, reproductive history, hormone therapy, and breast interventions (e.g., surgery or radiation) were also recorded to refine the analysis.
Over the follow-up period, 3,392 of these women experienced a first major cardiovascular event, including coronary artery disease, myocardial infarction, stroke, or heart failure. This significant event rate highlighted the imperative for more effective risk stratification methods in this population. The researchers developed a convolutional neural network, a form of deep learning, trained to extract and interpret complex patterns and features within mammographic images alongside the woman’s age to forecast the likelihood of a cardiovascular event within ten years.
Remarkably, the AI model’s predictive performance rivaled that of contemporary risk assessment tools such as New Zealand’s ‘PREDICT’ algorithm and the American Heart Association’s ‘PREVENT’ calculator, which both incorporate multifaceted clinical factors. Adding traditional clinical risk factors to the AI model slightly enhanced its accuracy, indicating that standard risk data may still have supplementary value. However, the AI’s ability to function effectively using only mammographic images and age underscores its potential as a standalone screening modality.
Several technical challenges and limitations were acknowledged by the researchers. Variability in image quality and characteristics due to different mammography scanners could affect the generalizability of the model across clinical settings. Furthermore, the comparative cardiovascular risk factors were self-reported, potentially introducing biases. The AI model’s performance inherently depends on the diversity and scope of its training data, raising questions about external validity in diverse populations beyond the Australian cohort.
Despite these caveats, the study’s most compelling advantage is its utilization of an already established screening infrastructure—routine mammography—which millions of women undergo worldwide. This ‘two-for-one’ screening concept offers significant efficiencies for both women and healthcare systems by capturing cardiovascular risk information without additional tests, medical visits, or data collection. Moreover, it presents a unique opportunity to elevate cardiovascular disease awareness among women, who historically perceive heart disease as a lesser threat compared to breast cancer.
In an editorial accompanying the study, experts from the University of Sydney emphasize the critical gap in cardiovascular risk recognition among women. They note that cardiovascular disease accounts for approximately 90% of deaths compared with breast cancer globally, a stark statistic that defies common public perceptions. They further suggest that mammography appointments could serve as vital ‘touchpoints’ to inform women about their heart health risks and potentially catalyze earlier interventions.
The embrace of machine learning for cardiovascular risk assessment is part of a growing trend in medical diagnostics and prognostics. However, translating these promising computational tools from research settings into routine clinical practice remains a significant hurdle. Implementation barriers include integrating AI algorithms with existing medical record systems, ensuring model transparency and interpretability, addressing ethical considerations, and securing regulatory approvals and clinician acceptance.
Ultimately, this study marks a pivotal step towards personalized cardiovascular risk screening tailored specifically for women, harnessing accessible imaging data in innovative ways. Ongoing refinement, broader validation in diverse populations, and concerted efforts to overcome implementation challenges will be essential to fully realize the potential of mammography-based machine learning for cardiovascular risk prediction. The convergence of medical imaging, AI, and preventive cardiology foreshadows a future where women’s heart health can be addressed proactively and efficiently within the framework of routine breast cancer screening programs.
Subject of Research: People
Article Title: Predicting cardiovascular events from routine mammograms using machine learning
News Publication Date: 16-Sep-2025
Web References: http://dx.doi.org/10.1136/heartjnl-2025-325705
Keywords: Cardiovascular disease, Mammography
Tags: AI algorithm for cardiovascular disease predictionAI in healthcare diagnosticsbiological differences in female heart diseasebreast arterial calcification and CVDcost-efficient cardiovascular risk detectiondual-purpose screening for womenenhancing women’s cardiovascular health managementinnovative healthcare solutions for CVDlimitations of traditional cardiovascular risk modelsroutine mammograms for heart disease riskunder-recognition of CVD risk in womenwomen’s health and cardiovascular risk assessment