Children with an inoperable type of brain cancer may benefit from an advanced immunotherapy treatment, according to new research.
Credit: Credit: WEHI researchers
Children with an inoperable type of brain cancer may benefit from an advanced immunotherapy treatment, according to new research.
At a glance
- Diffuse Intrinsic Pontine Glioma (DIPG) is an aggressive type of brain tumour that affects 20 children in Australia each year.
- WEHI researchers have found promise in treating DIPG with an innovative new immunotherapy treatment, called CAR T therapy.
- CAR T cells were able to enter the brain and have an anti-cancer effect by reducing the tumour burden in pre-clinical models.
Usually occurring in children aged five to seven years old, Diffuse Intrinsic Pontine Glioma (DIPG) is an aggressive type of brain tumour that affects 20 children in Australia each year.
The fast-growing tumour forms in the part of a child’s brain responsible for vital functions like breathing, swallowing and movement, meaning it is unable to be surgically removed.
Children diagnosed with DIPG are unlikely to survive a year beyond diagnosis and there is currently no treatment for this devastating condition.
CAR T therapy has anti-cancer effect on DIPG
WEHI researchers have found promise in treating DIPG with an innovative new immunotherapy treatment, called CAR T therapy.
Published in Neuro-Oncology Advances, the research showed CAR T therapy was effective at targeting DIPG tumours.
CAR T cell therapy involves isolating a patient’s immune cells, engineering them to become “super killer cells” and then re-infusing them into the patient to fight their cancer.
The research, led by Associate Professor Misty Jenkins, Laboratory Head at WEHI and The Brain Cancer Centre, showed in preclinical models these specifically-engineered CAR T cells were able to enter the brain and have an anti-cancer effect by reducing the tumour burden.
“Unlike radiation, which is a blunt instrument that kills cancerous as well as healthy brain tissue, CAR T cell therapy uses a patient’s own immune cells and engineers them to recognise and kill the tumour,” she said.
“CAR T cells offer a possibility of cure, with no long-term side-effects.
“These genetically-modified white blood cells act as a ‘living drug’, which means the patient will retain a living memory in their body of the anti-tumour response that may also work to kill the tumour again if it ever returns.
“The way these cells can completely eliminate the tumours and persist in the body into the future is what is so exciting about CAR T cell therapy, and why immunotherapy is the future of precision medicine.”
New target for future clinical trials
The study found DIPG brain tumours can be targeted using CAR T cells that recognise a cancer-specific protein called HER2. Once in the brain, the CAR T cells recognised this protein and signalled the T cells to kill the tumour cells.
Associate Professor Jenkins said the use of CAR T cell therapy had effectively eliminated the DIPG tumours in the study’s preclinical models.
“This paper shows that an approach to HER2 does work, and we hope to see this treatment incorporated into current and future clinical trials available to children in Australia,” she said.
“While there are no long-term studies yet, this research builds on other work that has shown this treatment to be effective in reducing DIPG tumours and improving the quality of life for these patients, who currently have no treatment options.
“Our hope is that this treatment will be included in future clinical trials and will eventually be used in combination with other drugs to treat DIPG.”
Laying the groundwork for new therapies
The research was a promising step forward in treating DIPG, Associate Professor Jenkins said.
“This lays the groundwork for us to interrogate thousands of potential therapies for anti-cancer immune cells to fight DIPG,” she said.
“Other studies have demonstrated this treatment approach is safe in children, so we are hopeful it won’t be long before it is clinically available.”
The research was made possible in part by funding from the Victorian Paediatric Cancer Consortium, Isabella & Marcus Foundation, Robert Connor Dawes Foundation and The Brain Cancer Centre.
The study, “HER2 Chimeric Antigen Receptor T cell immunotherapy is an effective treatment for Diffuse Intrinsic Pontine Glioma”, is published in Neuro-Oncology Advances (DOI: 10.1093/noajnl/vdad024).
WEHI authors: Stacie Wang, Alexander Davenport, Melinda Iliopoulos, Hannah Hughes-Parry, Katherine Watson, Valeria Arcucci, Matthias Mulazzani, Ryan Cross and Misty Jenkins.
Image Captions
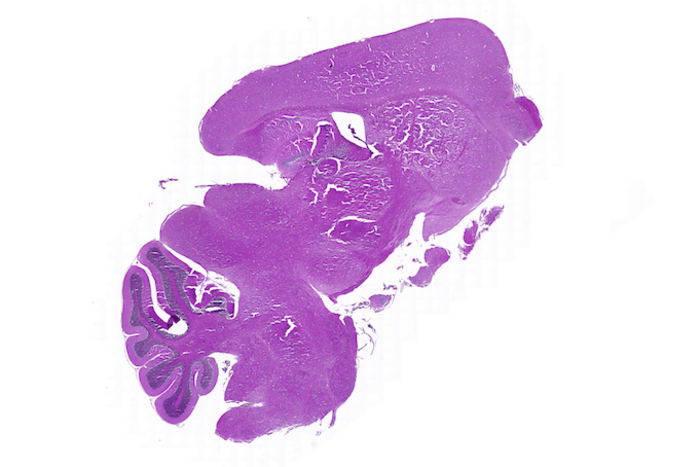
Tissue_sample
A histological image of a tissue sample studied in the research, which found the CART T cells persisted in the preclinical models post treatment, acting as a ‘living drug’ to fight the tumour if it returns.
Credit: WEHI researchers
WEHI_researchers
L-R: Mr Alex Davenport, Associate Professor Misty Jenkins, Dr Stacie Wang and Ms Melinda Iliopoulos.
Credit: WEHI
Immunotherapy infographic
CAR T cell therapy involves isolating a patient’s immune cells, engineering them to become “super killer cells” and then re-infusing them into the patient to fight their cancer.
Credit: WEHI
Journal
Neuro-Oncology Advances
DOI
10.1093/noajnl/vdad024
Method of Research
Observational study
Subject of Research
Animals
Article Title
HER2 chimeric antigen receptor T cell immunotherapy is an effective treatment for diffuse intrinsic pontine glioma
Article Publication Date
5-May-2023



