Scientists associated with the University of the Witwatersrand, Johannesburg are part of an international team that today published research suggesting a cure for HIV
Credit: Professor Annemarie Wensing, University Medical Center Utrecht, Netherlands
Scientists found no rebound of HIV in two patients who stopped taking their HIV medication after they received stem cell transplants for a hematological [blood] disease. Both patients underwent stem cell transplantation as part of their cancer treatment.
The transplanted donor cells had a gene defect [CCR5delta32mutant] which results in the absence of one of the critical entry gatekeepers that HIV generally needs to infect cells.
Thus far, only one person in the world – Timothy Ray Brown, known in 2008 as the ‘Berlin patient’ – has been cured of HIV. Although Brown had traces of HIV, the virus never rebounded and he is now celebrating 12 years’ cured of HIV.
Transplanted cells from a CCR5delta32 donor most likely protected Brown’s immune system. He also received aggressive chemotherapy, total body irradiation, and two stem cell transplants. For over a decade, the HIV field has puzzled over which of these factors were essential for his cure.
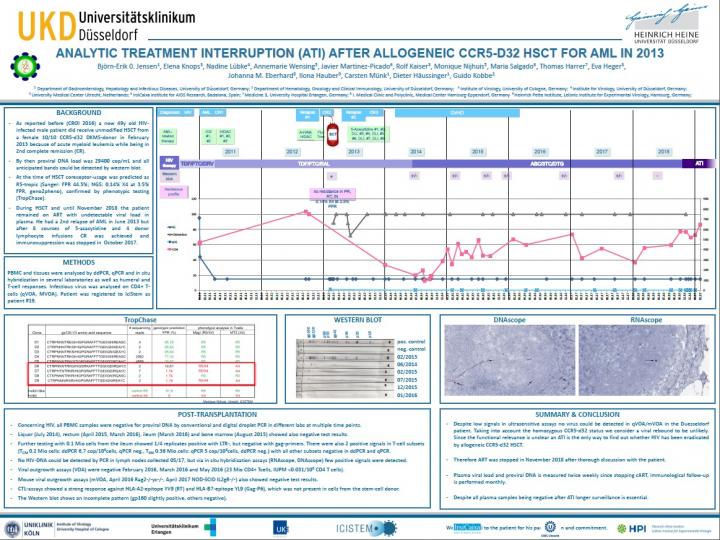
Groundbreaking research on the ‘London patient’ and the ‘Düsseldorf patient’ was presented at the Conference on Retroviruses and Opportunistic Infections, in Washington, 4-7 March 2019, and published in Nature.
Professor Ravi Gupta of University College London and the University of Cambridge presented a potential cure of HIV after stem cell transplantation in his ‘London patient’, while Dr. Björn Jensen from Düsseldorf University found his ‘Düsseldorf patient’ similarly potentially cured.
The London patient has not experienced HIV rebound during the 18 months since he stopped taking his antiviral medication. This is the longest adult HIV remission after stem cell transplantation since the Berlin patient.
The Düsseldorf patient stopped his HIV medication for a shorter period of just three-and-a-half months, but has also remains HIV free. Using the most sensitive techniques available to date, only traces of HIV DNA were detected.
The London and Düsseldorf patients show that after a single transplant and with even mild cancer chemotherapy and without radiation, remission may be achieved.
Both the London patient and the Düsseldorf patient were registered with the IciStem programme. IciStem is the International Collaboration to guide and investigate the potential for HIV cure by Stem Cell Transplantation.
Two IciStem scientific investigators in the London patient and Düsseldorf patient cases are also honorary full professors at the University of the Witwatersrand, Johannesburg (Wits). Annemarie Wensing is an Honorary Full Professor at the Wits Reproductive Health and HIV Institute (Wits RHI) and Professor Monique Nijhuis is an Honorary Full Professor in the HIV Pathogenesis Research Unit (HPRU) in the Faculty of Health Sciences at Wits. Both scientists hold primary appointments at the University Medical Center Utrecht in the Netherlands.
“Although delta32 donors are primarily found in Caucasian people, the London patient long-term remission case gives important insights into the potential mechanisms of cure and should fuel development of strategies that can be more broadly applied,” says Wensing.
IciStem has the largest programme to investigate HIV cure following stem cell transplantation. More than 22 000 donors with the rare CCR5delta32 gene defect have been identified and there are currently 39 patients registered with IciStem who have received transplants.
“To be clear, this is not an option yet for people with HIV, even in very rich countries, but it is a major step forward. This is incredibly exciting, as it furthers our understanding of the complex immunology of HIV and should get us closer to a cure,” says Professor Francois Venter, Deputy Executive Director, Wits RHI.
“Wits’ collaboration with Utrecht has been a delight and we have the combined expertise of Wits and Utrecht to do innovative work and conduct translational research that is published in top medical journals.”
One such collaboration is an HIV autopsy study funded by the South African Medical Research Council (SAMRC). The Strategic Health Innovation Partnerships (SHIP) grant for HIV Cure aims to identify the latent HIV reservoir in various body compartments and research the anatomical location and composition of the viral reservoir. The HIV reservoir is a major barrier to HIV Cure.
“We are using our experience from previous local autopsy studies and the tools developed in IciStem to perform rapid and in-depth post-mortem sampling through minimally invasive autopsies on recently deceased HIV-positive patients who were virologically suppressed or unsuppressed,” says Professor Maria Papathanasopoulos, SHIP principal investigator and director of the HPRU in the Department of Molecular Medicine and Haematology at Wits.
Professors Wensing and Nijhuis are part of SHIP along with Wits scientists Professors Neil Martinson, Caroline Tiemessen, Ebrahim Variava, and Francois Venter, and Doctors Adriaan Basson and Tanvier Omar.
“The London patient is the second HIV-positive man considered to be in prolonged remission after a bone marrow transplant from a CCR5 negative donor. This represents a critical moment in our search for an HIV cure. It reaffirms our belief that one day it will be possible to cure HIV infection with a safe, cost-effective, and easily accessible strategy,” says Papathanasopolous.
###
Media Contact
Deborah Minors
[email protected]
Original Source
http://www.




