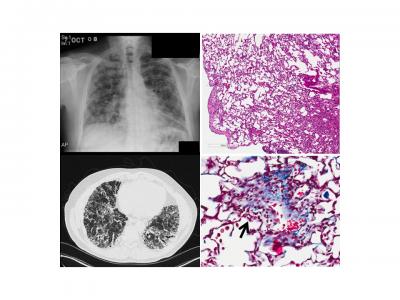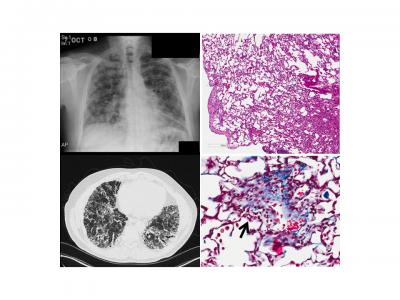
Credit: Michael Beers, Perelman School of Medicine, University of Pennsylvania
PHILADELPHIA–The biggest hurdle to finding effective therapies for idiopathic pulmonary fibrosis (IPF) – a life-threatening condition in which the lungs become scarred and breathing is increasingly difficult – has been the inability to fully model the disease in animals, limiting the ability to observe and understand the disease. Now, a team of researchers from Penn Medicine has developed the first mouse model with an IPF-associated mutation, which induces scarring and other damage similar to what is observed in humans suffering from the condition. The findings are published this week in the Journal of Clinical Investigation.
"No one has been able to make a model to date that actually mirrors what's going on in humans," said senior author Michael F. Beers, MD, a professor of Pulmonary, Allergy, and Critical Care in the Perelman School of Medicine at the University of Pennsylvania, and research director of the Penn Interstitial Lung Disease Center. "Now, we have a model that resembles the pathology, physiology, and molecular signs found in patients, which will allow us to work out new pathways and targets, and test drugs in more clinically relevant ways."
IPF, often caught in the mid to later stages, is diagnosed in about 50,000 people a year in the United States, and kills nearly 40,000 people during that same time. While there is no cure, two U.S. Food and Drug Administration-(FDA) approved drugs are used to slow the disease's progression, and some patients receive lung transplants. The median survival rate is two to three years from the time of diagnosis.
Current IPF mouse models rely on a chemotherapy drug to induce an "inflammatory storm" in the lungs that creates lesions about 21 days later, Beers said. But that doesn't reflect the process that actually occurs when humans develop the disease.
In the new mouse model, the team altered a gene for making a protein called surfactant protein-C (SFTPC), which is essential for lung function. Mutations in the SFTPC gene, which are found in certain human lung cells called alveolar epithelial cells (AECs), are a promising lead for homing in on one cause of the disease.
Knowing the importance of these lung AECs in the development of the disease, the team induced the SFTPC mutation into the AECs of normal mice to elicit a response. Within three days of inducing mutant SFTPC expression in adult mice, lung tissue was infiltrated by inflammatory cells; this was followed by an abnormal accumulation of inflammatory cells within tiny air sacs in the lungs. Rapid death was also observed in 30 to 50 percent of the animals. Similar to what has been observed in patients, the surviving mice went on to develop progressive fibrosis and loss of lung function.
Using the new animal model, the researchers will next look at pathways that lead to the initiation and persistence of lung fibrosis. "Now the questions become, why are those epithelial cells attracting both inflammatory cells and fibrotic cells? And how do these different cells talk to each other?" Beers said.
"We're also taking a big data approach by profiling the genetic, proteomic, and inflammatory changes in the mice over different time points," Beers added. "You can't do that in humans because we see these patients once their disease has already progressed. We know very little about what happens in the beginning. This model will help answer some of those questions and hopefully lead to more effective therapeutic drugs to slow the disease."
###
The research was conducted in collaboration with a translational research group consisting of both clinicians, including Namrata B. Patel, MD, clinical director of the Interstitial Lung Disease program, and Maryl Kreider MD, MSCE, director of the Interstitial Lung Disease program and scientists from the Penn Center for Pulmonary Biology and the Paul F. Harron Lung Center at Penn. Additional co-authors of the study include Shin-Ichi Nureki, Yaniv Tomer, Alessandro Venosa, Jeremy Katzen, Scott J. Russo, Sarita Jamil, Matthew Barrett, Vivian Nguyen, Meghan Kopp, and Surafel Mulugeta.
The study was supported by the Veterans Administration Merit Review (R01BX001176) and the National Institutes of Health (R01 HL119436, HL129150, 2T32 HL007586.).
Penn Medicine is one of the world's leading academic medical centers, dedicated to the related missions of medical education, biomedical research, and excellence in patient care. Penn Medicine consists of the Raymond and Ruth Perelman School of Medicine at the University of Pennsylvania (founded in 1765 as the nation's first medical school) and the University of Pennsylvania Health System, which together form a $7.8 billion enterprise.
The Perelman School of Medicine has been ranked among the top medical schools in the United States for more than 20 years, according to U.S. News & World Report's survey of research-oriented medical schools. The School is consistently among the nation's top recipients of funding from the National Institutes of Health, with $405 million awarded in the 2017 fiscal year.
The University of Pennsylvania Health System's patient care facilities include: The Hospital of the University of Pennsylvania and Penn Presbyterian Medical Center — which are recognized as one of the nation's top "Honor Roll" hospitals by U.S. News & World Report — Chester County Hospital; Lancaster General Health; Penn Medicine Princeton Health; Penn Wissahickon Hospice; and Pennsylvania Hospital – the nation's first hospital, founded in 1751. Additional affiliated inpatient care facilities and services throughout the Philadelphia region include Good Shepherd Penn Partners, a partnership between Good Shepherd Rehabilitation Network and Penn Medicine, and Princeton House Behavioral Health, a leading provider of highly skilled and compassionate behavioral healthcare.
Penn Medicine is committed to improving lives and health through a variety of community-based programs and activities. In fiscal year 2017, Penn Medicine provided $500 million to benefit our community.
Media Contact
Karen Kreeger
[email protected]
215-459-0544
@PennMedNews
http://www.uphs.upenn.edu/news/