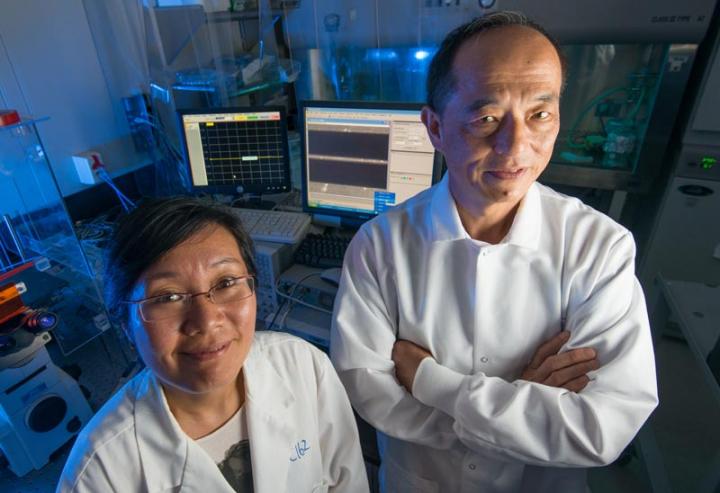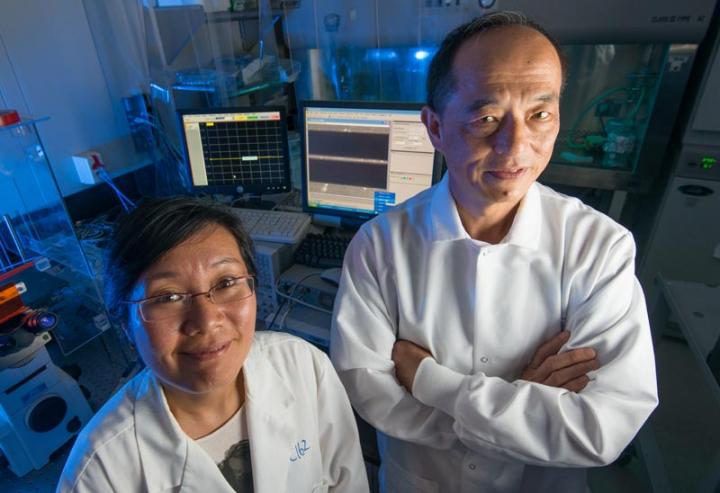
Credit: Lehigh University
To test for malignancy or monitor the effectiveness of cancer treatment, a person's tissue must be extracted, sent to a lab, stained and analyzed by a pathologist–a process that can take days to complete and is subject to human error.
Xuanhong Cheng, associate professor of materials science and engineering, and James Hwang, professor of electrical engineering and computer science, have something different in mind.
These two Lehigh University engineers are envisioning a future where cancer screening and treatment monitoring will be conducted at the point of care using microwave technology to characterize the nucleus of a single cell captured on a small microfluidic device. This lab-on-a-chip method would not only have the advantage of being portable, but would also be faster, cheaper, and more streamlined than currently available methods. The duo were recently awarded a three-year grant by National Science Foundation (NSF) to explore this unique approach.
Cheng and Hwang's technology begins with a microfluidic device that can capture–and then release–a single cell.
"The device works similarly to a person going through airport security," Cheng explains. "You are contained briefly, get scanned and then step out. In our device, a cell is held briefly, analyzed and released."
"Once a cell is captured, microwave technology is able to penetrate into the cell", says Hwang, "to sense what is inside."
"High-frequency microwave has the advantage of being able to penetrate through the cell and into the nucleus, like an x-ray is able to do for the human body, but without harming the cell." explains Cheng.
Cheng and Hwang intend to create the microwave equivalent of optical coherence tomography for single cell depth profiling to reveal intracellular details such as changes in nuclear morphology and DNA content.
They are building on their previous work that uses microwave technology to detect cell viability, in which they used their technique to characterize the cytoplasm surrounding the nucleus in a cell in order to differentiate between live and dead cells.
"The nucleus of abnormal cells look different than normal ones," says Cheng. "Normal cells tend to have fairly uniform morphology with a consistent nucleus to cytoplasm ratio. The nuclei of abnormal cells can be larger or smaller than normal cells, or are bizarrely shaped."
Now, Cheng and Hwang want to refine their technology to be able to characterize–or "see"–what is inside the nucleus.
They are working to advance both their hardware to achieve greater detection sensitivity, and their software to create more detailed computer models. They are also looking to experiment with using an array of sensors.
Hwang, an expert in microwave technology and computer modeling, believes they can do it.
"We've been successful with this technology," says Hwang. "Now, we want to move forward by one step to achieve a high enough resolution to separate the nucleus from the cytoplasm."
The team are doing basic research that could enable real-time dynamic monitoring of a cell nucleus, and contribute to fundamental understanding of cell development and malignancy progression.
###
Media Contact
Lori Friedman
[email protected]
610-758-3224
@lehighu
http://www.lehigh.edu