Neuherberg, April 27, 2016. Researchers at Helmholtz Zentrum München describe how breast cancer cells challenged with a small-molecule inhibitor targeting specific invasive properties switch to an alternative mode-of-action, rendering them even more aggressive. The results may impair future therapeutic approaches in the TGF-beta pathway and are published in the journal Oncotarget.
As breast cancer develops, tumor cells begin to breach the tissue compartment that normally confines the mammary gland and actively invade and spread into the surrounding tissue. The research team, led by Dr. Christina Scheel attempted to block this process by exposing cancer cells to a small-molecule inhibitor targeting the TGF-beta Receptor Type I (TGFBR1). TGFBR1 is a crucial relay-protein in a signaling cascade known to endow breast cancer cells with the ability to invade.
Indeed, by doing so the scientist of the Institute of stem cell research were able to prevent a master regulator of genes involved in this process from initiating a cellular program that results in invasive behaviour of cancer cells. This master regulator, Twist1, has long been implicated in breast cancer progression, but constitutes a type of protein that is currently not amenable to therapeutic targeting. Therefore, the researchers aimed to inhibit other, targetable signaling pathways that Twist1 depends on in order to mediate invasiveness.
Surprising results reveal the adaptiveness of breast cancer cells
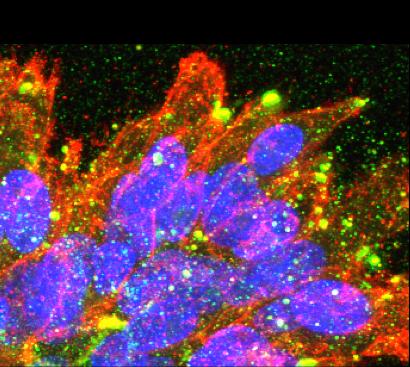
"Initially, using conventional in vitro tissue culture techniques, our results indicated that we were indeed successful, as many of the previously described effects of Twist1-activation were prevented by simultaneously blocking TGFBR1" says Diana Dragoi, PhD student at ISF and first author on the study. However, when the researchers transferred the breast cancer cells to a more physiological, 3D-environment, they discovered to their great surprise that Twist1 was able to render breast cancer cells invasive even while TGFBR1 signaling was blocked.
The breast cancer cells had simply switched to an alternative mode of invasion, spreading through the 3D-environment as cohesive strands of cells, instead of single cells. Moreover, these cells had significantly higher rates of proliferation, suggesting they were better equipped to launch secondary tumors after disseminating to distant sites. This latter process, termed metastasis, is the major course of morbidity for breast cancer patients: systemic dissemination and subsequent growth of breast cancer cells in vital organs such as the brain, bone marrow or liver eventually leads to their destruction.
"Taken together, our study suggests that the inhibition of TGFBR1 does not simply block the ability of master regulator Twist1 to induce invasiveness in breast cancer cells, but redirects the actions of Twist1 to generate breast cancer cells that may be even more aggressive" adds co-author Anja Krattenmacher (ISF). "These data highlight the importance of diligent preclinical tests that aim to approximate in vivo conditions as much as possible and to test many different parameters. This is especially important when aiming to interfere with such a complex, multi-step process as metastasis" concludes Dr. Scheel. In the complexity of breast cancer progression, the devil is in the detail.
###
Further Information
Background: About 70.000 Women are diagnosed with breast cancer every year in Germany alone. Despite significant progress in treatment, rapid adaptation in some aggressive subtypes of breast cancer causes therapeutic resistance and relapse. Therefore, elucidating how breast cancer cells adapt to therapeutic intervention is crucial for the development of effective treatment strategies.
Original Publication: Dragoi D. et al. (2016). Twist1 induces distinct cell states depending on TGFBR1-activation, Oncotarget, DOI: 10.18632/oncotarget.8878
The Helmholtz Zentrum München, the German Research Center for Environmental Health, pursues the goal of developing personalized medical approaches for the prevention and therapy of major common diseases such as diabetes and lung diseases. To achieve this, it investigates the interaction of genetics, environmental factors and lifestyle. The Helmholtz Zentrum München is headquartered in Neuherberg in the north of Munich and has about 2,300 staff members. It is a member of the Helmholtz Association, a community of 18 scientific-technical and medical-biological research centers with a total of about 37,000 staff members. http://www.helmholtz-muenchen.de/en/index.html
The Institute of Stem Cell Research (ISF) investigates the basic molecular and cellular mechanisms of stem cell maintenance and differentiation. From that, the ISF then develops approaches in order to replace defect cell types, either by activating resting stem cells or by re-programming other existing cell types to repair themselves. The aim of these approaches is to stimulate the regrowth of damaged, pathologically changed or destroyed tissue. http://www.helmholtz-muenchen.de/en/isf/index.html
Media Contact
Department of Communication, Helmholtz Zentrum München – German Research Center for Environmental Health, Ingolstädter Landstr. 1, 85764 Neuherberg – Tel: +49-89-3187-2238 – Fax: 089-3187-3324 – E-Mail: [email protected]
Scientific Contact at Helmholtz Zentrum München
Dr. Christina Scheel, Helmholtz Zentrum München – German Research Center for Environmental Health, Institute of Stem Cell Research, Independent Junior Group Mammary Stem Cells. Ingolstädter Landstr. 1, 85764 Neuherberg, Germany – Tel +49-89-3187-2012 – E-Mail: [email protected]
Media Contact
Dr. Christina Scheel
[email protected]
49-893-187-2012
http://www.gsf.de
The post Breast cancer progression — the devil is in the detail appeared first on Scienmag.





