Credit: Children's National Health System
WASHINGTON – (Jan. 4, 2018) – In pregnancies complicated by fetal congenital heart disease (CHD), global placental perfusion was significantly decreased and regional variation of placental perfusion significantly increased as pregnancies progressed, findings that point to non-invasive imaging providing an early warning of placental dysfunction. A Children's National Health System research team is thought to be the first to report non-invasive, whole placenta perfusion imaging in utero in a study published online Nov. 23, 2017 in Scientific Reports.
According to the National Heart, Lung and Blood Institute, congenital heart defects are the most common type of birth defect, affecting 8 in 1,000 newborns. Early in pregnancy, the fetal heart follows a parallel developmental course as the placenta, which supplies the growing fetus with oxygen and nutrients while ferrying out waste products. The study authors write that placental arteries are dynamic during pregnancy, remodeling themselves to accommodate increased blood flow as fetuses undergo explosive growth spurts in later stages of pregnancy. If this crucial remodeling does not occur, the placenta may not supply sufficient oxygen and nutrients to the fetus, leading to fetal growth restriction or preeclampsia.
The research team led by Catherine Limperopoulos, Ph.D., enrolled 48 pregnant women who underwent at least one fetal magnetic resonance imaging (MRI) session during their second or third trimester of pregnancy. Thirty-one of the women were healthy volunteers whose mean gestational age was 30 weeks (range: 21 to 39 gestational weeks). Seventeen women were pregnant with fetuses diagnosed with CHD whose mean gestational age was 32 weeks (range: 22 to 38 gestational weeks).
The researchers used velocity-selective arterial spin labeling (VSASL), a powerful MRI technique that directly measures the rate of delivery of arterial blood to organs like the brain. ASL tracks water molecules within the blood as blood flows through arteries, eliminating the need to use a contrast agent. The team was able to distinguish the placenta perfusion contributions by the fetus and the mother.
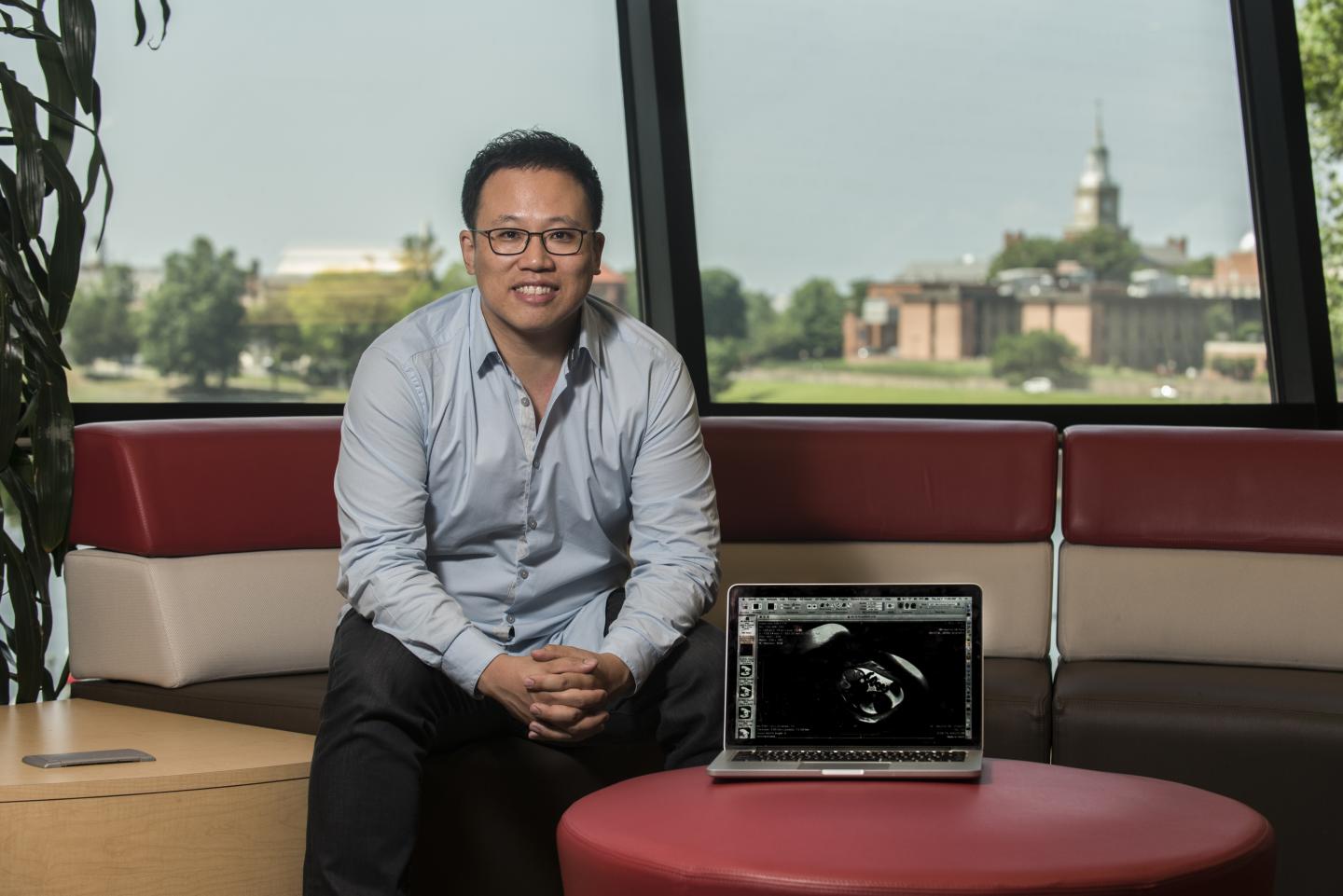
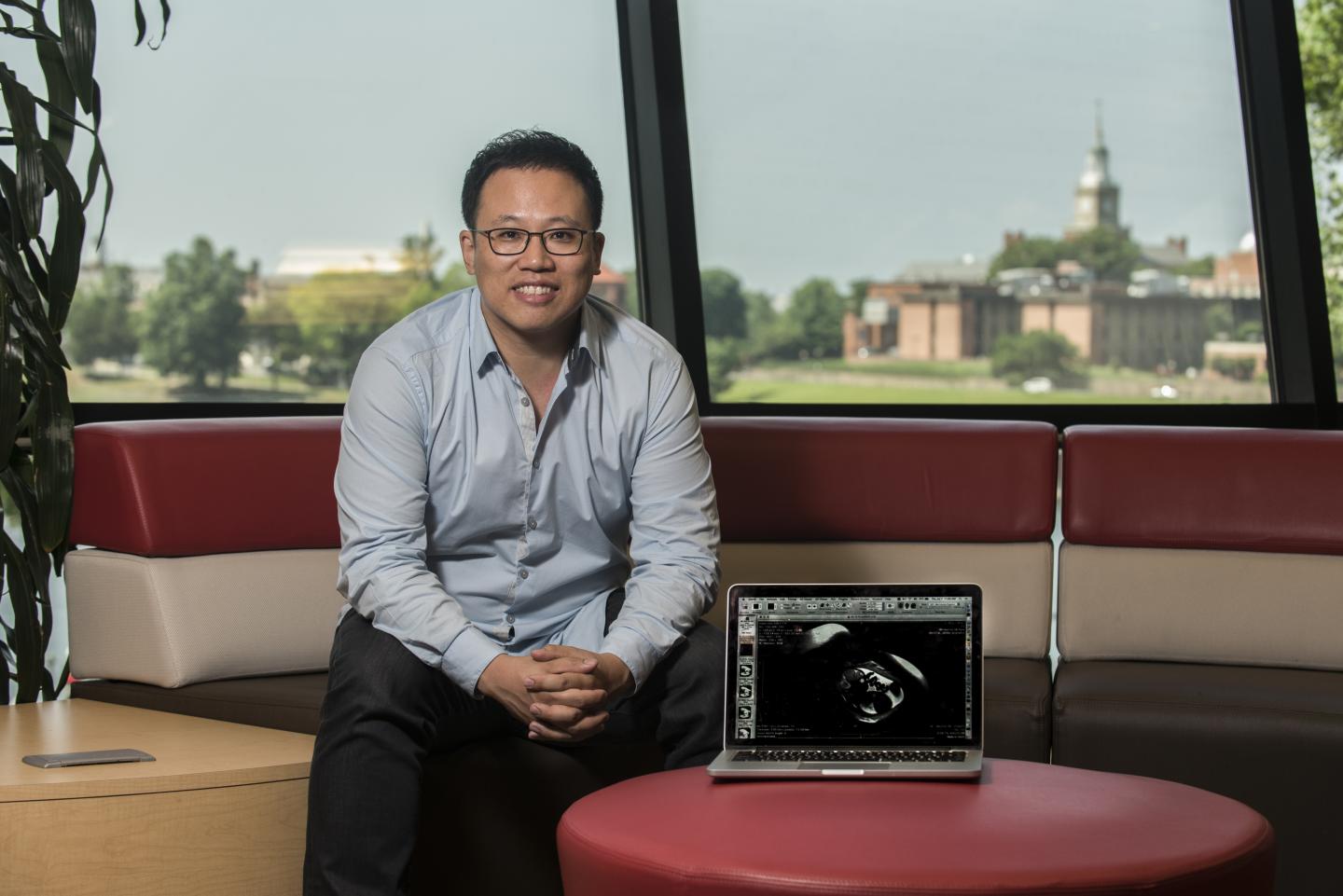
"In pregnancies complicated by fetal CHD, global placental perfusion significantly decreased and regional variation of placental perfusion significantly increased with advancing gestational age," says Zungho "Wesley" Zun, Ph.D., the study's lead author.
"Just like the human brain, heart and kidneys–organs that can commandeer heightened blood flow when needed–the placenta may employ an auto-regulatory mechanism to optimize perfusion," adds Limperopoulos, director of Children's Developing Brain Research Laboratory and the study's senior author. "The early increased global placental profusion in pregnancies complicated by CHD may represent an attempt to correct for insufficient fetal blood flow."
The research team writes that the findings demonstrate that placental dysfunction due to CHD can be apparent as early as the second trimester of pregnancy using this imaging technology.
"The predictive value of VSASL imaging, which we continue to study, holds the promise of detecting dysfunction before placental abnormalities become irreversible," Limperopoulos says.
###
In addition to Zun and Limperopoulos, Children's National study co-authors include Neonatologist Nickie N. Andescavage, M.D., and Cardiologist Mary T. Donofrio, M.D. The other member of the study team is Greg Zaharchuk, M.D., Ph.D., of Stanford University.
Research reported in this news release was supported by the National Heart, Lung and Blood Institute of the National Institutes of Health (NIH) under award number R01 HL116585-01 and the National Center for Advancing Translational Sciences of the NIH under award numbers UL1TR000075 and KL2TR000076.
Media Contact
Diedtra Henderson
[email protected]
443-610-9826
http://www.childrensnational.org/
Related Journal Article
http://dx.doi.org/10.1038/s41598-017-16461-8