Credit: SY Cho, EJ Lipson, H Im, et al., Johns Hopkins University School of Medicine, Baltimore, MD
RESTON, Va. – Advanced melanoma, a type of skin cancer that has spread to other areas of the body, has a poor prognosis, but immune checkpoint inhibitor therapy can be effective for some patients. Research highlighted in the featured article of the September issue of The Journal of Nuclear Medicine demonstrates that combined positron emission tomography/computed tomography (PET/CT) scanning early in treatment could identify whether the therapy will benefit a particular patient. As the therapy has potentially serious side-effects, early determination of ineffectiveness could avert unnecessary risk exposure and provide the option of a different treatment.
Immune checkpoint inhibitors (ICI) block certain proteins made by immune system cells, such as T cells, and some cancer cells that were keeping the immune system's T cells from killing the cancer cells. When these checkpoint proteins are blocked by inhibitors, the immune system can function again and T cells are better able to destroy cancer cells.
Determining response to ICI therapy has been challenging. "Current anatomic CT-based response criteria are typically performed at the earliest two to four months into treatment and are limited in their ability to assess stable disease and pseudoprogression," explains Steve Y. Cho, MD, one of the lead authors of this prospective study funded by the Melanoma Research Alliance and conducted at Johns Hopkins University School of Medicine, Baltimore, Maryland, with Richard L Wahl, MD and in close collaboration with melanoma specialists Evan Lipson, MD, and Suzanne Topalian, MD. Hyung Jun Im, MD, is also a major contributor to this study with Cho, who is now at the University of Wisconsin School of Medicine and Public Health, Madison, Wisconsin.
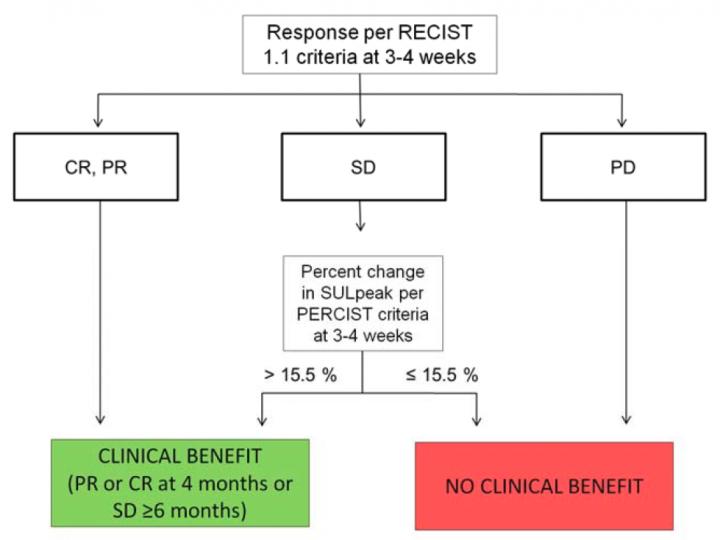
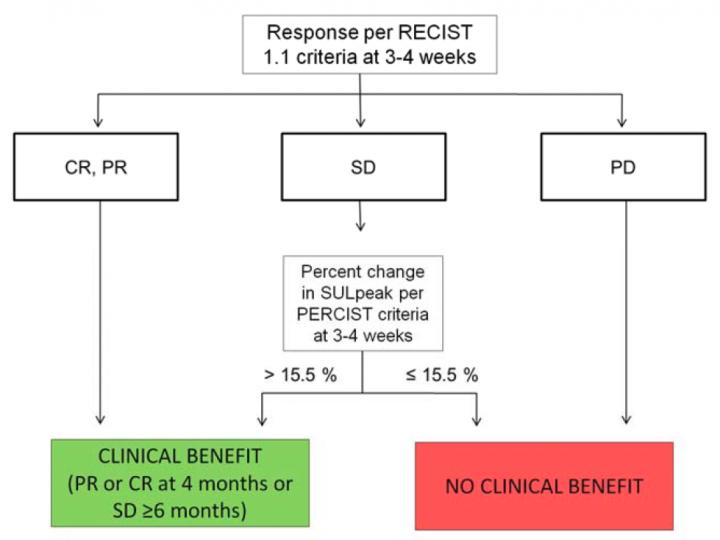
The study evaluated the use of 18F-fluorodeoxyglucose-(FDG)-PET/CT scanning as an early predictor of response to ICI therapy in 20 patients with advanced melanoma. The patients each had three scans: prior to treatment, at 21 to 28 days and at four months. The researchers developed criteria to predict eventual response to ICI with 100% sensitivity, 93% specificity and 95% accuracy.
Cho notes, "When 18F-FDG PET-based response criteria were combined with CT-based criteria, we were able to more accurately differentiate eventual clinical benefit. Based on our data, we have proposed a combined PET and CT-based response criteria to immune-checkpoint inhibitor therapy in advanced metastatic melanoma. Interestingly, we found a small increase in 18F-FDG tumor uptake at this early time point that may implicate an active immune mediated 'flare' as a good indication that the tumor is responsive to the immune therapy."
He cautions, "While immune therapies, including the particular class of immune checkpoint inhibitors used in this study, promise new hope for durable tumor responses and remission for a variety of cancers, they are not without a cost. The same immune cells triggered to attack cancer cells can also attack normal organs, causing immune-related adverse events, which can limit the continued use of these agents. Therefore, early discontinuation of these therapies can limit the risk for side effects and allow for initiation of other more effective treatment options." The next step is for further studies with larger cohorts.
The National Institutes of Health states that more than 1 million people in the U.S. are living with melanoma and estimates that in 2017 more than 87,000 new cases of melanoma will be diagnosed, and the cancer will cause nearly 10,000 deaths. According to the American Cancer Society, the five-year survival rate for individuals with stage 4 melanoma is only about 15 to 20 percent.
Looking ahead, Cho points out, "Incorporation of more effective and early PET- and CT-based response assessment criteria could also be used to more optimally assess novel emerging immune-based therapies in drug development for melanoma and other tumors."
###
The authors of "Prediction of Response to Immune Checkpoint Inhibitor Therapy Using Early Time-Point FDG-PET/CT Imaging in Patients with Advanced Melanoma" include Steve Y. Cho, Johns Hopkins University School of Medicine and Sidney Kimmel Comprehensive Cancer Center, Baltimore, Maryland, and currently the University of Wisconsin School of Medicine and Public Health and Carbone Comprehensive Cancer Center, Madison, Wisconsin; Hyung-Jun Im, University of Wisconsin School of Medicine and Public Health and Carbone Comprehensive Cancer Center, Madison, Wisconsin; Evan J. Lipson, Steven P. Rowe, Esther Mena Gonzalez, Amanda Blackford, Alin Chirindel, Drew M. Pardoll, and Suzanne L. Topalian, Johns Hopkins University School of Medicine and Sidney Kimmel Comprehensive Cancer Center, Baltimore, Maryland; and Richard L. Wahl, Johns Hopkins University School of Medicine and Sidney Kimmel Comprehensive Cancer Center, Baltimore, Maryland, and currently the Mallinckrodt Institute of Radiology, Washington University School of Medicine, St. Louis, Missouri.
Please visit the SNMMI Media Center to view the PDF of the study, including images, and more information about molecular imaging and personalized medicine. To schedule an interview with the researchers, please contact Laurie Callahan at (703) 652-6773 or [email protected]. Current and past issues of The Journal of Nuclear Medicine can be found online at http://jnm.snmjournals.org.
About the Society of Nuclear Medicine and Molecular Imaging
The Society of Nuclear Medicine and Molecular Imaging (SNMMI) is an international scientific and medical organization dedicated to raising public awareness about nuclear medicine and molecular imaging, a vital element of today's medical practice that adds an additional dimension to diagnosis, changing the way common and devastating diseases are understood and treated and helping provide patients with the best health care possible.
SNMMI's more than 15,000 members set the standard for molecular imaging and nuclear medicine practice by creating guidelines, sharing information through journals and meetings and leading advocacy on key issues that affect molecular imaging and therapy research and practice. For more information, visit http://www.snmmi.org.
Media Contact
Laurie Callahan
[email protected]
@SNM_MI
http://www.snm.org
Original Source
http://www.snmmi.org/NewsPublications/NewsDetail.aspx?ItemNumber=25198 http://dx.doi.org/10.2967/jnumed.116.188839