Researchers have devised a novel cancer treatment that destroys tumor cells by first disarming their defenses, then hitting them with a lethal dose of DNA damage.
In studies with mice, the research team showed that this one-two punch, which relies on a nanoparticle that carries two drugs and releases them at different times, dramatically shrinks lung and breast tumors. The MIT team, led by Michael Yaffe, the David H. Koch Professor in Science, and Paula Hammond, the David H. Koch Professor in Engineering, describe the findings in the May 8 online edition of Science Signaling.
“I think it’s a harbinger of what nanomedicine can do for us in the future,” says Hammond, who is a member of MIT’s Koch Institute for Integrative Cancer Research. “We’re moving from the simplest model of the nanoparticle — just getting the drug in there and targeting it — to having smart nanoparticles that deliver drug combinations in the way that you need to really attack the tumor.”
Doctors routinely give cancer patients two or more different chemotherapy drugs in hopes that a multipronged attack will be more successful than a single drug. While many studies have identified drugs that work well together, a 2012 paper from Yaffe’s lab was the first to show that the timing of drug administration can dramatically influence the outcome.
In that study, Yaffe and former MIT postdoc Michael Lee found they could weaken cancer cells by administering the drug erlotinib, which shuts down one of the pathways that promote uncontrolled tumor growth. These pretreated tumor cells were much more susceptible to treatment with a DNA-damaging drug called doxorubicin than cells given the two drugs simultaneously.
“It’s like rewiring a circuit,” says Yaffe, who is also a member of the Koch Institute. “When you give
the first drug, the wires’ connections get switched around so that the second drug works in a much more effective way.”
Erlotinib, which targets a protein called the epidermal growth factor (EGF) receptor, found on tumor cell surfaces, has been approved by the Food and Drug Administration to treat pancreatic cancer and some types of lung cancer. Doxorubicin is used to treat many cancers, including leukemia, lymphoma, and bladder, breast, lung, and ovarian tumors.
Staggering these drugs proved particularly powerful against a type of breast cancer cell known as triple-negative, which doesn’t have overactive estrogen, progesterone, or HER2 receptors. Triple-negative tumors, which account for about 16 percent of breast cancer cases, are much more aggressive than other types and tend to strike younger women.
That was an exciting finding, Yaffe says. “The problem was,” he adds, “how do you translate that into something you can actually give a cancer patient?”
From lab result to drug delivery
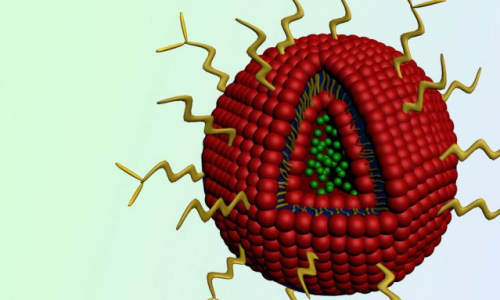
To approach this problem, Yaffe teamed up with Hammond, a chemical engineer who has previously designed several types of nanoparticles that can carry two drugs at once. For this project, Hammond and her graduate student, Stephen Morton, devised dozens of candidate particles. The most effective were a type of particle called liposomes — spherical droplets surrounded by a fatty outer shell.
The MIT team designed their liposomes to carry doxorubicin inside the particle’s core, with erlotinib embedded in the outer layer. The particles are coated with a polymer called PEG, which protects them from being broken down in the body or filtered out by the liver and kidneys. Another tag, folate, helps direct the particles to tumor cells, which express high quantities of folate receptors.
Once the particles reach a tumor and are taken up by cells, the particles start to break down. Erlotinib, carried in the outer shell, is released first, but doxorubicin release is delayed and takes more time to seep into cells, giving erlotinib time to weaken the cells’ defenses. “There’s a lag of somewhere between four and 24 hours between when erlotinib peaks in its effectiveness and the doxorubicin peaks in its effectiveness,” Yaffe says.
The researchers tested the particles in mice implanted with two types of human tumors: triple-negative breast tumors and non-small-cell lung tumors. Both types shrank significantly. Furthermore, packaging the two drugs in liposome nanoparticles made them much more effective than the traditional forms of the drugs, even when those drugs were given in a time-staggered order.
“This [particle delivery system] not only provides a platform for time-staggered treatment strategies in cancer, but also for delivering the drugs more directly to the tumor tissue itself,” says Rune Linding, a professor of systems biology at the Technical University of Denmark who was not part of the research team. “The latter is vital, as one of the major drawbacks of traditional chemotherapy is the general wipeout of normal cells in the patient’s body, dramatically weakening the patient and worsening survival and response to treatment.”
As a next step before possible clinical trials in human patients, the researchers are now testing the particles in mice that are genetically programmed to develop tumors on their own, instead of having human tumor cells implanted in them.
The researchers believe that time-staggered delivery could also improve other types of chemotherapy. They have devised several combinations involving cisplatin, a commonly used DNA-damaging drug, and are working on other combinations to treat prostate, head and neck, and ovarian cancers. At the same time, Hammond’s lab is working on more complex nanoparticles that would allow for more precise loading of the drugs and fine-tuning of their staggered release.
“With a nanoparticle delivery platform that allows us to control the relative rates of release and the relative amounts of loading, we can put these systems together in a smart way that allows them to be as effective as possible,” Hammond says.
Story Source:
The above story is based on materials provided by MIT News Office, Anne Trafton.