In a groundbreaking study published in the Journal of Translational Medicine, researchers led by Ji, Z., He, M., and Wu, H., have unveiled pivotal insights into the mechanisms underlying vascular restenosis. This phenomenon, often occurring after vascular injuries such as angioplasty, has long posed formidable challenges in cardiovascular medicine. With the potential implications of their findings, the team highlights a novel avenue for therapeutic intervention that targets macrophage pyroptosis, a form of programmed cell death that plays a key role in inflammation and tissue repair.
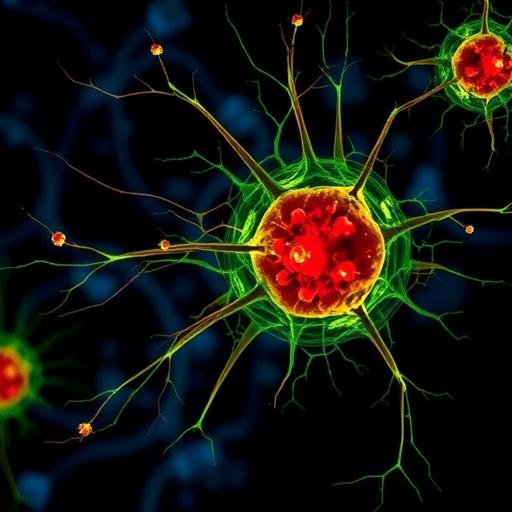
Macrophages, integral to the immune response, exhibit diverse functional states, including pro-inflammatory and anti-inflammatory phenotypes. Their role in wound healing and tissue repair is critical, yet the processes they invoke can have paradoxical effects. Inflammation, while necessary for initial repair, can lead to excessive fibrosis and neointimal hyperplasia when uncontrolled. This fine balance underscores the importance of understanding macrophage behavior during the healing process, especially following vascular injuries.
In their research, the authors meticulously investigated how inhibiting macrophage pyroptosis affects neointimal formation and restenosis. Pyroptosis, characterized by cell swelling, membrane rupture, and the release of inflammatory cytokines, amplifies local inflammation. The study articulated that when macrophages undergo pyroptosis, they can inadvertently exacerbate inflammation and tissue remodeling, giving rise to complications such as restenosis.
To delve into their hypothesis, the researchers employed an array of experimental models, including in vitro assays and in vivo interventions utilizing rodent models of vascular injury. Through these methodologies, they assessed the impact of pharmacological agents designed to inhibit pyroptosis, monitoring subsequent alterations in macrophage behavior and vascular remodeling processes. Remarkably, the findings indicated that the inhibition of pyroptosis not only mitigated inflammation but also significantly reduced neointimal thickness, suggesting a promising therapeutic strategy for enhancing vascular healing.
The study shines a light on the duality of macrophage functions in the vascular environment. While traditionally viewed as mere inflammatory mediators, these cells possess versatile roles that influence not just inflammation but overall vascular health. By harnessing the knowledge of macrophage biology, particularly in relation to pyroptosis, researchers can pave the way for innovative treatments that eschew the shortcomings of conventional therapies.
Moreover, this understanding resonates well with the evolving field of regenerative medicine, where the aim is not only to treat but also to repair and regenerate damaged tissues. By specifically targeting macrophage pyroptosis, clinicians may soon have a strategic tool at their disposal that modulates the immune response, effectively steering it towards a beneficial outcome post-injury.
In concert with these findings, the study emphasizes the significance of research in controlled inflammation and healing processes. Uncontrolled inflammation has been established as a key contributor to various pathologies, including atherosclerosis and restenosis. This study invites further exploration into precisely how macrophages orchestrate these responses and how they can be manipulated to foster a favorable healing environment.
The potential implications of this research extend beyond a single aspect of vascular intervention. Understanding macrophage behavior could revolutionize how we approach not only restenosis but a multitude of conditions characterized by aberrant inflammation and repair processes. From chronic wounds to vascular graft failures, the insights derived from inhibiting pyroptosis could provide a template for therapeutic development across various medical arenas.
Importantly, the researchers noted the necessity for future studies to validate these findings across different models and humanized systems. While the initial results are promising, a broader understanding encompassing varied biological contexts will be essential for transitioning these findings from bench to bedside. The translational potential of this research underscores the importance of interdisciplinary collaboration, merging insights from immunology, cardiology, and regenerative medicine to foster innovative approaches to patient care.
As cardiovascular diseases remain a leading cause of morbidity and mortality worldwide, the urgency for novel therapeutic strategies has never been clearer. The findings from Ji, Z., He, M., and Wu, H. represent a beacon of hope in this relentless pursuit. Enhanced understanding of macrophage pyroptosis could attribute to significant improvements in the quality of life for countless patients undergoing vascular interventions.
Finally, this study is not merely an academic exercise; it is a clarion call for a paradigm shift in how we understand inflammation and healing. The potential to reprogram the immune response, particularly within the context of vascular health, could lead to transformative changes in both clinical practice and patient outcomes. As more researchers dive deeper into the intricacies of macrophage behavior, the broader implications of these findings will continue to unfold, sparking further advancements in the treatment of vascular disorders.
In conclusion, the work of Ji et al. stands as a critical step towards unraveling the complexities of vascular healing. By putting macrophage pyroptosis under the microscope, they have not only addressed a relevant clinical issue but also opened new avenues for therapeutic exploration. The move towards harnessing innate immune mechanisms to improve vascular outcomes represents a progressive leap forward in medical science, with the potential to reshape the landscape of cardiovascular therapeutics for years to come.
Subject of Research: Macrophage pyroptosis inhibition in vascular restenosis.
Article Title: Macrophage pyroptosis inhibition alleviates postinjury neointimal formation and vascular restenosis.
Article References: Ji, Z., He, M., Wu, H. et al. Macrophage pyroptosis inhibition alleviates postinjury neointimal formation and vascular restenosis. J Transl Med (2026). https://doi.org/10.1186/s12967-026-07777-z
Image Credits: AI Generated
DOI: 10.1186/s12967-026-07777-z
Keywords: Macrophage pyroptosis, neointimal formation, vascular restenosis, inflammation, therapeutic strategies, cardiovascular medicine.
Tags: angioplasty complicationscardiovascular medicine challengesfibrosis and inflammation balanceimmune response in wound healinginflammation and tissue repairmacrophage functional statesmacrophage pyroptosis inhibitionneointimal hyperplasia preventionprogrammed cell death in macrophagestherapeutic interventions in vascular diseasestranslational medicine research.vascular restenosis mechanisms