In the relentless quest to enhance precision and efficiency in radiation therapy, a team of researchers led by Professor Fu Jin has pioneered an innovative hybrid approach that synergizes Monte Carlo (MC) simulation with deep learning techniques to revolutionize patient-specific quality assurance (QA). This breakthrough hinges on solving a fundamental trade-off that has long challenged the field: obtaining high-accuracy dosimetric verification without incurring prohibitive computational delays. As radiation therapy becomes increasingly adaptive and personalized, especially in modalities like online adaptive radiation therapy (ART), the demand for swift, reliable dose verification intensifies. Professor Fu Jin’s team has addressed this critical clinical bottleneck by combining the cutting-edge power of GPU-accelerated MC code ARCHER with the sophisticated noise-suppressing capabilities of the SUNet deep neural network.
EPID (Electronic Portal Imaging Device) systems are now integral to real-time in vivo dose verification due to their capacity to measure transmitted radiation doses during therapy sessions. Yet, despite their clinical benefits, the use of MC simulations to model EPID response remains computationally expensive. MC simulation, esteemed as the “gold standard” in dose calculation, inherently requires simulating an immense number of particle histories to minimize stochastic noise and achieve high-fidelity results. Increasing particle counts from millions to billions ensures accuracy but causes exponential blows to calculation speed, making real-time dose verification impractical. On the other hand, reducing particle numbers introduces significant noise artifacts, compromising the integrity of dose measurements and rendering them unsuitable for clinical decision-making.
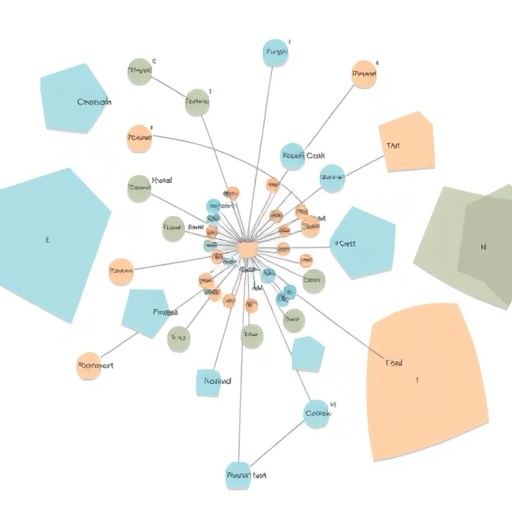
This inherent tension motivated the research team to devise a hybrid MC-deep learning framework that harnesses both computational strengths. The framework capitalizes on the GPU-accelerated ARCHER Monte Carlo simulation to rapidly generate EPID transmission dose data, albeit with noise arising from reduced particle counts. To denoise these outputs without monopolizing computational resources, the deep learning model SUNet—an advanced neural network architecture tailored for image denoising—was employed. Lung cancer intensity-modulated radiation therapy (IMRT) cases served as the testbed, where four distinct data sets were generated using differing particle histories: 1 million, 10 million, 100 million, and 1 billion particles.
The training methodology is particularly notable for its rigor. Using the 1 billion-particle data set as the gold standard, the SUNet network learned to reconstruct high-quality dose distributions from the noisy, low-particle simulations. By supervising the model on this highest-fidelity output, the researchers effectively taught SUNet to interpolate missing and corrupted information from lower-particle noisy inputs, thereby achieving a remarkable balance between speed and accuracy. This denoising process proved to be exceptionally fast, requiring only a fraction of a second per image, which is transformative considering the traditionally extensive runtimes associated with pure Monte Carlo calculations.
Quantitatively, the gains are striking. Processing data initially simulated with a mere 1 million particles, the denoised outputs saw the structural similarity index measure (SSIM)—a standard metric evaluating image fidelity—jump from 0.61 to an impressive 0.95. Simultaneously, the gamma passing rate (GPR), a clinical metric for dosimetric accuracy, soared from below 50% to over 89% post-denoising. For the optimal 10 million-particle data set, the performance improved further, achieving an SSIM of 0.96 and a GPR exceeding 94%, balancing the needs of clinical accuracy and computational feasibility. Even at the 100 million-particle level, closer to traditional standards of precision, denoising nudged the GPR to nearly 99.6%, indicative of near-perfect dose agreement. Moreover, the denoising step’s brevity—averaging only 0.13 to 0.16 seconds—reduced the overall computational time drastically; 1.88 seconds for the 10 million-particle data and 8.76 seconds for the 100 million-particle data, times unheard of for such detailed Monte Carlo analyses.
Visually, the denoised images shed the grainy noise characteristic of low-particle MC simulations, revealing smooth dose profiles that faithfully preserved critical anatomical and clinical features. This visual clarity is paramount not only for physician confidence but also for automated verification systems that increasingly rely on robust image and dose modulations. The practical implications are profound, as QA processes that once took tens of minutes or longer can now be integrated into near real-time clinical workflows, providing oncologists with timely feedback to adjust treatment plans on the fly.
The significance of this advancement resonates particularly in the context of online adaptive radiation therapy (ART), a domain where patient anatomy and tumor positions evolve between treatment fractions and even during a single session. Rapid verification of delivered doses is essential in ART to promptly adapt plans, maintain treatment efficacy, and reduce adverse effects. The integrated MC-DL framework meets this demanding clinical scenario by furnishing a versatile computational strategy: the 10 million-particle setting balances rapid turnaround with sufficient accuracy for routine adaptive QA, while the 100 million-particle level serves high-precision needs for complex cases.
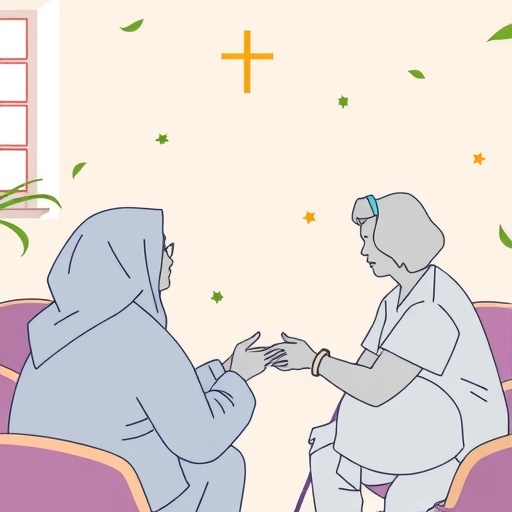
Professor Fu Jin summarized the innovation as a marriage between the venerable accuracy of Monte Carlo physics-based modeling and the transformative speed of deep learning, yielding a tool that is not only theoretically elegant but clinically actionable. Such technology stands to advance radiation oncology workflows beyond current benchmarks, laying the groundwork for future endeavors like three-dimensional dose reconstructions and extension of QA protocols across diverse tumor sites and treatment machines. Importantly, the approach represents a shift towards intelligent QA systems that leverage AI for dose prediction enhancement, promising to democratize advanced radiation therapy worldwide.
Looking forward, the research team envisions refining the SUNet architecture further to achieve even greater denoising efficiency and exploring alternative neural networks that might provide complementary strengths in dose modeling. There is also interest in expanding the methodology to encompass additional treatment sites beyond lung cancer, including head and neck, prostate, and pediatric cancers, thereby broadening the clinical impact. Integrating multi-modal imaging data and patient-specific anatomical changes into the model could also pave the way for personalized, adaptive dose verification paradigms that push the envelope of cancer treatment safety and effectiveness.
This pioneering study was published in the journal Nuclear Science and Techniques on January 29, 2026, signaling a significant leap in quality assurance protocols in radiation oncology. As emerging technologies continuously reshape cancer care, the fusion of physics-based simulation with cutting-edge artificial intelligence provides a beacon of innovation, promising faster, more accurate, and ultimately safer treatments for patients everywhere.
Subject of Research: Not applicable
Article Title: A novel method for EPID transmission dose generation using Monte Carlo simulation and deep learning
News Publication Date: 29-Jan-2026
Web References:
10.1007/s41365-026-01898-2
Image Credits: Tao Qiu
Keywords: Radioactive decay, Radiation therapy
Tags: adaptive radiation therapy advancementsbreakthroughs in radiation therapy technologycomputational efficiency in dosimetric verificationdeep learning for dose verificationEPID systems in radiation therapyGPU-accelerated Monte Carlo methodsinnovative hybrid approaches in medical physicsMonte Carlo simulation in radiation therapynoise-suppressing neural networks in medical imagingpatient-specific quality assurance in oncologyprecision medicine in radiation oncologyreal-time in vivo dose measurement