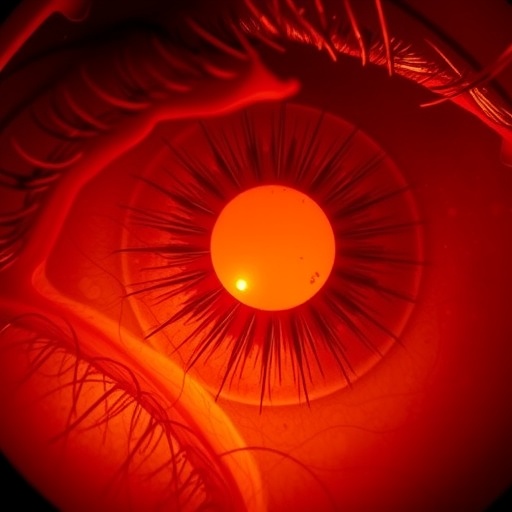
Diabetic retinopathy represents a silent epidemic that continues to threaten the vision of millions of people worldwide. As the incidence of diabetes climbs steadily, the complications associated with it, most notably diabetic retinopathy (DR), emerge as a pressing public health concern. In their recent study, Tang, Jiang, Sun, and colleagues shine a light on the often-overlooked aspects of this condition, delving deep into the reasons behind its varying severity among individuals. What sets certain patients on a path to more severe outcomes? The answer is intricately tied to retina-specific risk factors and a phenomenon referred to as metabolic memory.
Understanding diabetic retinopathy requires grappling with its complex pathophysiology. At the heart of DR is the deleterious effect of hyperglycemia on retinal vasculature. Prolonged high blood sugar levels induce a series of biochemical changes that culminate in ischemia and inflammation, causing damage to the neuronal cells and retinal pigment epithelium. This cascade sets the stage for the development of both non-proliferative and proliferative forms of diabetic retinopathy. By exploring these underlying mechanisms, the research team offers insights that can help galvanize innovative therapeutic strategies aimed at arresting or even reversing the progression of this sight-threatening condition.
A cornerstone of the research is the exploration of retina-specific risk factors. While systemic factors such as duration of diabetes, hypertension, and dyslipidemia have traditionally been viewed as instrumental in the development of DR, the researchers emphasize that the retina’s unique anatomy and physiology can dramatically alter the pathway to disease. The retinal microenvironment, characterized by its limited capacity for regeneration and a distinct enzootic composition, plays a pivotal role in determining how diabetes actually manifests in retinal tissues. For instance, inflammatory cytokines that contribute to retinal neuronal death may be more abundant in certain individuals, influencing their susceptibility to severe disease.
Furthermore, metabolic memory emerges as a critical theme in this investigation. The concept posits that the effects of hyperglycemia are not merely transient; rather, they leave behind a lasting imprint that can affect retinal health long after glucose levels have been normalized. The research highlights how prior exposure to elevated blood sugar can lead to epigenetic changes within retinal cells, predisposing them to future complications. This understanding implies that proactive management of blood glucose levels is not just about immediate outcomes—it’s about safeguarding long-term retinal integrity.
By focusing on these crux concepts, the authors provide a valuable framework for anticipating the risks associated with diabetic retinopathy. They argue for a paradigm shift in how clinicians approach diabetes management, advocating for tailored strategies that consider individual susceptibility beyond traditional risk stratifications. This could include personalized screening regimens that prioritize individuals who, based on their retinal risk profiles, may require more intensive monitoring and intervention.
An equally compelling dimension of this research is how it delineates the interplay between genetic predispositions and environmental factors. While genetics undoubtedly set the stage for an individual’s risk profile, environmental elements such as diet, lifestyle, and even access to healthcare resources play a crucial role in modulating that risk. The researchers underscore the necessity of an integrated approach that encompasses both genetic research and epidemiological studies to fully understand the multifaceted nature of diabetic retinopathy.
Moreover, the study reveals the dire need for increased awareness around diabetic retinopathy, particularly in communities disproportionately affected by diabetes. Preventative measures and education around recognizing the symptoms of DR can be lifesaving, especially in populations where access to healthcare is limited. Heightened awareness can facilitate earlier intervention, thus improving overall patient outcomes and reducing the burden of visual impairment among diabetic individuals.
With these insights, the authors argue that future research must pivot toward multifaceted interventions that target not only the modulation of blood glucose levels but also address specific retinal vulnerabilities. From a therapeutic standpoint, efforts such as the development of neuroprotective agents, anti-inflammatory drugs, and even gene therapy approaches could hold promise for transforming the landscape of treatment options available for DR.
In closing, this research not only elucidates the complexities surrounding diabetic retinopathy but also serves as a clarion call to the scientific and medical communities. By advancing our understanding of the retina’s specific risk factors and the long-term implications of metabolic memory, we position ourselves to better confront the ugly realities of diabetic retinopathy. As awareness grows and research delves deeper, there is hope on the horizon for those facing the daunting challenge of preserving vision in the wake of diabetes.
This study’s findings underscore the importance of personalized medicine in the management of diabetic retinopathy. Tailoring treatment plans to individual profiles will not only enhance patient outcomes but may also facilitate advancements in our therapeutic arsenal against this sight-threatening condition. The integration of cutting-edge research with clinical endeavors promises to usher in a new era in the fight against diabetic retinopathy.
In summary, the ongoing journey of discovery in diabetic retinopathy highlights the need for interdisciplinary collaboration. By bringing together expertise from fields ranging from genetics to clinical practice, researchers and healthcare providers can collectively craft a more informed and effective approach to preventing significant vision loss among diabetic patients. Ultimately, embracing this multifaceted strategy will be essential to combat one of the most severe complications that arise from diabetes.
As Tang, Jiang, Sun, and their team continue to pave the way for future research, their work stands as a testament to the indelible link between scientific inquiry and real-world health outcomes. In addressing the challenges posed by diabetic retinopathy, we inch closer to delivering the promise of preserved vision for millions affected by diabetes, championing a future where individuals can visualize their lives without the shadow of sight impairment clouding their hopes and dreams.
Subject of Research: Diabetic retinopathy and its retinal-specific risk factors.
Article Title: Diabetic retinopathy: why some eyes suffer more – a focus on retina-specific risk factors and metabolic memory.
Article References:
Tang, S., Jiang, L., Sun, W. et al. Diabetic retinopathy: why some eyes suffer more – a focus on retina-specific risk factors and metabolic memory.
J Transl Med (2026). https://doi.org/10.1186/s12967-025-07622-9
Image Credits: AI Generated
DOI: 10.1186/s12967-025-07622-9
Keywords: diabetic retinopathy, metabolic memory, retina-specific risk factors, personalized medicine, diabetes management, vision loss.
Tags: diabetic complications and preventiondiabetic retinopathy risk factorshyperglycemia effects on visioninnovative therapeutic strategies for DRischemia and inflammation in retinopathymetabolic memory in diabetesnon-proliferative diabetic retinopathypathophysiology of diabetic retinopathyproliferative diabetic retinopathypublic health concerns diabetesretinal vasculature damagevision loss from diabetes