In an impressive stride towards enhancing prenatal diagnostics, a new study led by Huynh and colleagues explores the relevance of measuring fetal endometrial thickness as a pivotal method for diagnosing ovarian cysts in unborn children. This non-invasive approach opens a new frontier in prenatal care, promising to refine how clinicians assess potential complications involving the ovaries of the developing fetus.
The research paper, soon to be published in Pediatric Radiology, delves deep into the intricate dynamics of prenatal diagnostics. One of the principal questions the study seeks to address is the relationship between fetal endometrial thickness and the presence of ovarian cysts. Understanding this relationship is crucial as it could significantly ease the anxiety surrounding unexpected findings during routine ultrasounds, ultimately leading to more informed clinical decisions.
Endometrial thickness in fetuses has often been overlooked as a diagnostic tool. The authors argue that measuring this variable may reveal important insights into the health of fetal ovaries and indicate potential pathologies, particularly concerning ovarian cysts. These cysts, while often benign, can lead to complications if not monitored appropriately. The study’s innovative approach offers a fresh perspective; it paves the way for improved monitoring strategies that can mitigate risks associated with ovarian conditions in neonates.
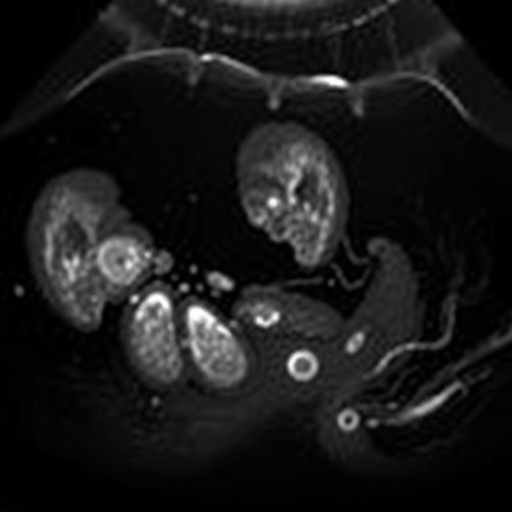
The methodology employed in the study encompassed a robust observational framework involving a substantial cohort of expectant mothers undergoing routine imaging. The researchers meticulously analyzed ultrasound images to measure endometrial thickness accurately. To bolster the reliability of their findings, they adopted advanced imaging techniques that enhance clarity, thereby enabling a more precise assessment of endometrial and ovarian anatomy.
The results of the research were promising. A statistically significant correlation emerged between measured endometrial thickness and the incidence of ovarian cysts during later visits. This connection holds merit, as it suggests that a simple measurement could serve as an early warning signal for potential complications that necessitate closer monitoring. Such findings could prove invaluable in clinical practice, allowing for pre-emptive interventions that could potentially save lives or mitigate complications.
Another critical aspect addressed in the study is the psychological impact on parents when faced with fetal anomalies detected via ultrasound. The authors highlight the emotional turmoil families endure when confronted with uncertain outcomes. By unveiling a reliable indicator—endometrial thickness—that can signal the presence of concerning conditions, this research may help alleviate some of that anxiety for expectant parents.
Moreover, the researchers underscore the need for ongoing education for sonographers and clinicians in recognizing and interpreting fetal endometrial measurements. Recommendations for curriculum enhancements emphasize the critical role this measurement can play in ultrasound assessments. This pivotal knowledge shift has the potential to transform current ultrasound protocols and introduce a paradigm change in how fetal health is evaluated.
The implications for practice extend beyond just diagnosis. The study’s findings could foster a more proactive approach to monitoring fetal health. Clinicians could implement protocols that involve regular assessments of endometrial thickness, allowing for early detection of ovarian cysts and timely management strategies. Such proactive monitoring is essential in ensuring the well-being of both mother and child, creating a safety net that reassures families during pregnancy.
It is essential to acknowledge the limitations of the study as well. While the findings are revolutionary, the researchers point out that further longitudinal studies are needed to solidify these conclusions. The dynamics of fetal development are complex, and additional research will help delineate other influencing factors on endometrial thickness and cyst development. Thus, while the results are promising, they are just the beginning of an exciting exploration into fetal health diagnostics.
In conclusion, this groundbreaking research represents a significant milestone in pediatric radiology. The assessment of fetal endometrial thickness emerges as a formidable tool for the prenatal diagnosis of ovarian cysts. By integrating this measurement into routine practices, healthcare providers can enhance their diagnostic capabilities and offer more comprehensive care to expectant mothers. As the medical community begins to embrace these findings, the future of prenatal diagnostics appears brighter, potentially transforming the landscape of fetal medicine.
The excitement surrounding this research reaffirms the essential role that innovative tools and techniques can play in enhancing patient care and advancing medical knowledge. The collaborative efforts of the authors and their commitment to improving outcomes for mothers and their unborn children are commendable. This study not only paves the way for improved healthcare practices but also exemplifies the power of research in addressing real-world clinical challenges.
As this work makes its way through the publication process, anticipation builds for its subsequent incorporation into clinical guidelines and educational programs. This holistic approach to fetal health could herald a new era of diagnostics that prioritizes safety and efficacy for the most vulnerable patients—unborn children.
In summary, Huynh and colleagues have illuminated a path forward through their insights into fetal endometrial thickness and its implications for prenatal diagnosis, ultimately shaping a legacy that might resonate within the medical community for years to come.
Subject of Research: Fetal endometrial thickness and its relation to ovarian cysts
Article Title: Assessment of fetal endometrial thickness: a key to the prenatal diagnosis of ovarian cysts
Article References:
Huynh, MH., De Leon Benedetti, L., Mathew, L. et al. Assessment of fetal endometrial thickness: a key to the prenatal diagnosis of ovarian cysts.
Pediatr Radiol (2026). https://doi.org/10.1007/s00247-025-06494-x
Image Credits: AI Generated
DOI: 23 January 2026
Keywords: Fetal health, endocrinology, ovarian cysts, prenatal diagnostics, ultrasound imaging.
Tags: complications of ovarian cysts in pregnancyendometrial thickness fetal assessmentfetal health monitoring strategiesfetal ovarian health assessmentsimproving clinical decision-making in pregnancynon-invasive prenatal care techniquesovarian cyst diagnosis in fetusespediatric radiology research findingsprenatal diagnostics advancementsrelationship between endometrial thickness and ovarian cystssignificance of ultrasound in prenatal careunderstanding fetal pathologies