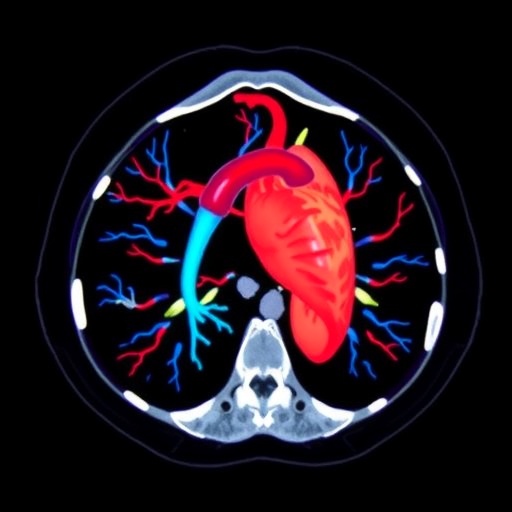
In the rapidly evolving field of pediatric cardiology, the role of computed tomographic angiography (CTA) has gained significant prominence. This imaging modality, particularly when utilizing photon-counting detectors, not only enhances the visual resolution of cardiovascular structures but also presents critical concerns regarding radiation exposure. As healthcare professionals adopt advanced imaging technologies, understanding the trade-offs between image quality and patient safety will become paramount. Recent research by Vijayasimha seeks to clarify these trade-offs, emphasizing the necessity for standardized protocols in the application of photon-counting detector technology in pediatric cardiac CTA.
At the heart of this inquiry is the recognition that children are inherently more susceptible to the harmful effects of radiation than adults. This vulnerability necessitates a cautious approach to diagnostic imaging, particularly in a population that is often undergoing repeated examinations. Pediatric patients possess a longer life expectancy, providing more time for potential adverse effects from radiation exposure to manifest. Thus, clinicians must balance the need for precise imaging with an acute awareness of radiation dosage during procedures.
Photon-counting detectors represent a breakthrough in imaging technology. Unlike conventional detectors that output a continuous analog signal, photon-counting devices register individual photons, resulting in enhanced signal-to-noise ratios and improved image quality. This technological enhancement allows for lower radiation doses while preserving diagnostic accuracy. However, as noted by Vijayasimha, there remains a critical gap in standard protocols for utilizing these detectors, particularly in pediatric cardiology, where both the accuracy of images and the health of young patients are of utmost importance.
Vijayasimha’s comprehensive study makes a compelling case for the establishment of standardized imaging protocols that specifically address the unique needs of pediatric patients. Without clear guidelines, variability in radiation doses can occur, leading to either unnecessary exposure or inadequate imaging quality. By advocating for standardization, the research paves the way for improved outcomes in the realm of pediatric cardiac CTA.
The crux of the research emphasizes that while technological advancements enhance diagnostic capabilities, the absence of clear procedural protocols can lead to inconsistencies and increased risks. Medical practitioners, radiologists, and technologists will need to collaborate and create a framework that defines optimal practices for photon-counting detectors, thereby reducing the variability in radiation dose among different healthcare settings. This call for standardization is a clarion reminder that innovation in medical imaging must be coupled with responsible and uniform practices.
One of the specific areas of focus in Vijayasimha’s findings lies in the development of dose-optimization strategies. These strategies incorporate the principles of the ALARA (As Low As Reasonably Achievable) approach, which emphasizes minimizing radiation exposure while achieving necessary diagnostic information. By leveraging advanced algorithms and machine learning, medical imaging can evolve to provide optimal doses tailored to individual patient needs, particularly in pediatric populations where variability in body size and composition can significantly affect radiation absorption.
Another essential aspect of the study is the exploration of the educational components necessary for clinicians and imaging specialists. Training programs must include a robust curriculum on the implications of radiation exposure and the intricacies of photon-counting technology. By equipping healthcare professionals with knowledge and skills around dose management, the healthcare community can navigate the complexities of modern imaging with more confidence and efficacy.
Furthermore, the research highlights the need for future studies that explore the long-term outcomes of radiation exposure in pediatric patients undergoing CTA. Continuous monitoring and analysis will provide invaluable data to substantiate and refine the proposed standard protocols. This ongoing research is crucial, as it not only informs clinical practices but also shapes the legislative and ethical frameworks surrounding pediatric imaging.
Importantly, the implications of this research extend beyond clinical settings. Policymakers and regulatory bodies must take heed of the findings to establish guidelines that protect vulnerable populations from potential radiation hazards. By fostering an environment in which standardization is prioritized, the medical community can work towards delivering safe and effective imaging services that cater specifically to the pediatric cohort.
In conclusion, Vijayasimha’s research sheds light on a pressing issue within pediatric cardiology—the need for clear, standardized protocols in the use of photon-counting detectors in CTA. The study underscores the dual responsibility of advancing technology while ensuring patient safety, advocating for collaborative efforts among professionals in the field. The shockwaves of these findings resonate beyond individual practices, encouraging a holistic approach to pediatric imaging that prioritizes both innovation and care.
The future of pediatric cardiac imaging with photon-counting technology is indeed bright, provided we remain vigilant in our commitment to enhancing safety standards. As healthcare advances, so too must the methodologies that guide our practices, ensuring that we do not compromise on the proactive measures necessary to protect our youngest patients.
In facing the intertwined challenges of innovation and patient safety, the research by Vijayasimha stands as a vital contribution towards creating a balanced approach in pediatric cardiac CTA procedures. This research is a timely reminder of our obligations as medical professionals—not only to leverage the best technologies available but also to safeguard those who entrust us with their care.
Subject of Research: Photon-counting detector pediatric cardiac computed tomographic angiography
Article Title: Clarifying radiation-dose trade-offs in photon-counting detector pediatric cardiac computed tomographic angiography: protocol standardization as the missing variable.
Article References:
Vijayasimha, M. Clarifying radiation-dose trade-offs in photon-counting detector pediatric cardiac computed tomographic angiography: protocol standardization as the missing variable.
Pediatr Radiol (2026). https://doi.org/10.1007/s00247-025-06489-8
Image Credits: AI Generated
DOI: 19 January 2026
Keywords: Pediatric cardiology, photon-counting detectors, computed tomographic angiography, radiation exposure, protocol standardization, dose optimization, healthcare policy.
Tags: advanced imaging technologiescardiovascular imaging advancementsclinician awareness in imagingcomputed tomographic angiographylong-term effects of radiationpediatric cardiologypediatric diagnostic procedurespediatric imaging safetyphoton-counting detectorsradiation exposure in childrenstandardized imaging protocolstrade-offs in imaging quality