Leptomeningeal metastasis (LM) represents a formidable challenge in oncology, particularly among patients suffering from non-small cell lung cancer (NSCLC) with mutations in the epidermal growth factor receptor (EGFR). The intricacies associated with LM, arising from such mutations, have raised significant concerns regarding treatment protocols and patient outcomes. The growing understanding of the molecular mechanisms driving EGFR mutations has fostered advancements in therapeutic strategies, propelling researchers and clinicians toward new horizons in clinical medicine.
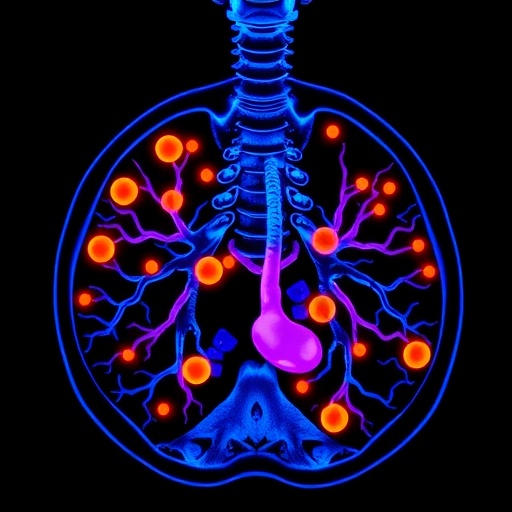
In recent years, it has become increasingly clear that EGFR mutations significantly affect the biology of lung cancer, resulting in distinct pathological features. These mutations alter tumor behavior, facilitate invasive properties, and intensify the likelihood of metastasis, especially to the leptomeninges— the delicate membranes surrounding the brain and spinal cord. The progression of EGFR mutant NSCLC to LM underscores the critical need to customize treatment regimens, as these patients exhibit specific clinical presentations that diverge from those with typical NSCLC.
The clinical landscape of treating leptomeningeal metastasis has evolved dramatically. Intrathecal therapy has emerged as a central tenet in addressing this particular manifestation of metastasis. The direct administration of therapeutic agents into the cerebrospinal fluid facilitates higher local drug concentrations and potentially mitigates systemic toxicity. Moreover, innovative intravenous therapies are being explored to enhance the drug’s efficacy while preserving neurological function, an essential consideration given the sensitive nature of brain tissues.
In reviewing the efficacy of target therapies specifically designed for EGFR mutations, researchers have made significant strides. The advent of third-generation EGFR tyrosine kinase inhibitors (TKIs) has revolutionized the treatment landscape. Drugs like osimertinib have shown remarkable promise in halting disease progression in patients who harbor certain mutations. This progress is crucial, as traditional chemotherapy has often proven inadequate against LM, prompting a shift towards more precision-based approaches in treatment.
Nevertheless, the therapeutic window for administering interventional measures remains limited. Timing is critical; delays in treatment can result in rapid disease progression and poorer prognoses. Thus, ongoing clinical trials exploring adaptive treatment algorithms are essential to ensure timely intervention. Monitoring biomarkers that signal LM onset, alongside the continual assessment of tumor response to therapy, are crucial elements in effective patient management.
As scientists delve into the molecular biology underpinning LM, they uncover pathways that may be targeted for future therapies. Recent studies illuminating the role of the tumor microenvironment have opened new avenues for therapeutic intervention. Factors influencing the blood-brain barrier’s permeability are receiving keen scrutiny, as enhancing drug delivery across this barrier could profoundly impact treatment success. Understanding these complex interactions fosters a more refined approach to developing drugs that can penetrate the central nervous system (CNS).
Despite these advancements, the clinical management of LM remains riddled with challenges. The symptoms patients experience, ranging from headache and cognitive decline to cranial nerve deficits, complicate the landscape of treatment. Healthcare providers must navigate these murky waters with awareness and sensitivity, as symptom management is as critical as controlling the disease itself. Collaborative approaches among multidisciplinary teams—oncologists, neurologists, and palliative care specialists—are essential in crafting a holistic pathway for patient care.
The survival rates for patients with leptomeningeal manifestations of EGFR mutant NSCLC are generally low, highlighting the need for continuous research and therapeutic advancements. Many studies aim to optimize existing therapies while exploring novel agents that could prove efficacious against LM. Immunotherapeutic approaches, harnessing the body’s immune system to combat tumor cells, are currently an area of intense investigation. The potential of chimeric antigen receptor (CAR) T-cell therapy and immune checkpoint inhibitors is being diligently explored for their ability to elicit robust antitumor responses.
Additionally, the importance of genetic profiling cannot be overstated. Personalized medicine, guided by specific genetic alterations within a tumor, paves the way for tailor-made treatment protocols. The unique mutations present in each patient’s tumor can direct clinicians to the most effective therapies and improve the chances of favorable outcomes. Genetic testing has become a vital component of the diagnostic process, enabling healthcare providers to stratify patients appropriately.
Patient education forms another critical pillar in managing leptomeningeal metastasis effectively. Empowering patients with knowledge about their disease process, treatment options, and potential side effects fosters better communication and adherence to complex therapeutic regimens. Engaging patients in shared decision-making ensures that treatment aligns with personal values and preferences, ultimately leading to enhanced satisfaction with care.
In summary, therapeutic progress in addressing leptomeningeal metastasis resulting from EGFR mutant non-small cell lung cancer marks an era of hopeful innovation and relentless research. The concerted efforts made by scientists and clinicians to unravel the underlying mechanisms of this condition will hopefully lead to improved treatment paradigms that enhance survival and quality of life for affected patients. As research continues to unfold, the landscape of LM will undoubtedly transform, affording those impacted by this devastating diagnosis a more hopeful outlook on life.
The delays in obtaining effective treatments underscore the urgent need for more extensive clinics and larger studies to accumulate robust data on treatment efficacy. Multicentric trials, designed to harness the collective experience of several centers, will play a pivotal role in validating novel treatments and elucidating their place in the current therapeutic arsenal. In a field as rapidly evolving as oncology, the potential fosters an exhilarating prospect for the future of patient care.
While the road ahead may be fraught with challenges, the synergy of cutting-edge research, technological advancements, and patient-centered care promises a new dawn in the management of leptomeningeal metastasis in EGFR mutant non-small cell lung cancer. The culmination of these efforts will not only enhance our collective understanding but also empower future generations of cancer care specialists to redefine the battle against this formidable foe.
Subject of Research: Leptomeningeal metastasis in EGFR mutant non-small cell lung cancer
Article Title: Therapeutic progress in leptomeningeal metastasis from EGFR mutant non-small cell lung cancer: a clinical medicine review
Article References:
Ding, T., Xie, Y. & Ding, M. Therapeutic progress in leptomeningeal metastasis from EGFR mutant non-small cell lung cancer: a clinical medicine review.
J Cancer Res Clin Oncol 152, 38 (2026). https://doi.org/10.1007/s00432-025-06416-2
Image Credits: AI Generated
DOI: https://doi.org/10.1007/s00432-025-06416-2
Keywords: EGFR mutations, non-small cell lung cancer, leptomeningeal metastasis, targeted therapy, treatment progress, clinical medicine.
Tags: cerebrospinal fluid drug administrationclinical outcomes for LM patientscustomized cancer treatment regimensEGFR mutations in lung cancerintrathecal therapy for metastasisinvasive properties of NSCLC mutationsLeptomeningeal metastasis treatmentmetastatic pathways in lung cancermolecular mechanisms of EGFR mutationsnon-small cell lung cancer advancementsoncological challenges in NSCLCtherapeutic strategies for leptomeningeal involvement