In a groundbreaking advance that could reshape the therapeutic landscape of pancreatic ductal adenocarcinoma (PDAC), researchers have unveiled how the drug Derazantinib significantly enhances the effectiveness of gemcitabine, a standard chemotherapy agent. This discovery centers around Derazantinib’s ability to suppress key signaling pathways—namely NF-κB and MAPK—that are known to drive cancer cell survival and drug resistance in PDAC, ultimately leading to a marked reduction in the expression of the mucin protein MUC5AC, which plays a critical role in tumor progression.
Pancreatic cancer remains one of the most lethal malignancies worldwide, with dismal five-year survival rates that have stubbornly resisted improvement despite decades of research. Gemcitabine, a nucleoside analog, has long been employed in treating PDAC, yet its clinical benefit is limited by intrinsic or acquired resistance mechanisms inherent to tumor cells. The molecular underpinnings of this chemoresistance have been a key focus in oncological research, aiming to uncover co-targets that could be modulated to potentiate gemcitabine’s efficacy.
The team led by Ye, W. and colleagues embarked on an in-depth investigation into the intracellular signaling milieu of PDAC cells treated with Derazantinib in combination with gemcitabine. Importantly, Derazantinib functions as an inhibitor of the fibroblast growth factor receptor (FGFR), a family of tyrosine kinase receptors implicated in the pathogenesis and progression of several cancers. In PDAC, aberrant FGFR signaling has been documented to promote oncogenic processes such as cellular proliferation, invasion, and survival, thereby representing a promising therapeutic target.
Through meticulous molecular analyses, the researchers uncovered that treatment with Derazantinib attenuated the activation levels of the NF-κB and MAPK pathways. NF-κB is a pivotal transcription factor orchestrating a broad array of cellular responses, including inflammation, apoptosis avoidance, and proliferation. Its hyperactivation is frequently associated with tumor aggressiveness and poor prognosis in pancreatic cancer. Similarly, the MAPK signaling cascade, which transduces extracellular growth signals into diverse cellular responses, is frequently deregulated in malignancies, facilitating oncogenic transformation and chemoresistance.
By dampening these pro-survival and pro-proliferative pathways, Derazantinib undermines the cellular defenses that PDAC cells typically mount against chemotherapeutic insult. One of the most striking findings from the study is the consequential suppression of MUC5AC expression. MUC5AC is a gel-forming mucin that constitutes a major component of the extracellular mucus barrier, and its overexpression in pancreatic tumors contributes to an environment conducive to tumor growth and metastasis, while simultaneously impairing drug delivery and efficacy.
Notably, the downregulation of MUC5AC serves a dual purpose: it dismantles the physical and biochemical shield that cancer cells exploit, and it simultaneously disrupts the signaling loops that sustain their malignant phenotype. This dual impact is hypothesized to underlie the observed enhancement of gemcitabine’s cytotoxic effects when co-administered with Derazantinib.
The implications of these insights are profound. First, they offer a mechanistic rationale for combining FGFR inhibitors with conventional chemotherapy to overcome resistance barriers in PDAC. Second, they provide a compelling example of the potential to modulate tumor microenvironment factors, such as mucins, to improve drug delivery and response. Finally, they underscore the intricate crosstalk between oncogenic signaling pathways and extracellular matrix components, shedding light on novel angles for therapeutic intervention.
The methodology employed in this study was comprehensive, encompassing both in vitro and in vivo models. PDAC cell lines exposed to the combinatory regimen exhibited significant reductions in cell viability relative to gemcitabine alone, validating the synergistic effect. Moreover, xenograft experiments in murine models confirmed the enhanced tumor growth suppression with Derazantinib and gemcitabine co-treatment. These findings provide strong translational potential for clinical application, highlighting a pathway to increase survival outcomes for PDAC patients.
One of the technical highlights involves the quantification of NF-κB and MAPK pathway activity via Western blot analysis and immunofluorescence staining. The study revealed that phosphorylation events critical to signal transduction were markedly diminished upon Derazantinib treatment. This biochemical attenuation translated into decreased nuclear localization and transcriptional activity of NF-κB, thereby weakening the expression of downstream anti-apoptotic genes.
Furthermore, transcriptomic analyses demonstrated a consistent downregulation of MUC5AC mRNA levels, corroborating the protein expression data and reinforcing the conclusion that Derazantinib exerts a suppressive effect at the transcriptional level. The data also suggest that MUC5AC downregulation may itself feed back to further inhibit the MAPK pathway, indicating a complex interdependence between these molecular players.
The study also addressed potential concerns regarding toxicity and off-target effects. The combined treatment was well-tolerated in preclinical models, with no significant weight loss or organ damage observed, indicating a favorable therapeutic index. This safety profile is crucial when considering the translation into clinical trials, as PDAC patients often suffer from treatment-associated morbidity that limits chemotherapy dosing.
Importantly, this research aligns with the growing paradigm shift towards combination therapies tailored to disrupt multiple facets of tumor biology simultaneously. By specifically targeting both cell-intrinsic signaling mechanisms and extracellular protective factors such as mucins, therapeutic regimens can potentially surmount the multifactorial barriers that have historically curtailed progress in pancreatic cancer treatment.
While the study primarily centers on the interplay between Derazantinib and gemcitabine, it also raises intriguing questions about the broader application of FGFR inhibitors in other mucin-overexpressing tumors, such as certain subtypes of lung and colorectal cancers. The molecular mechanisms delineated here may serve as a blueprint for exploring analogous combinatorial strategies in diverse oncologic contexts.
Looking forward, the translational momentum generated by these findings could catalyze early-phase clinical trials assessing the efficacy of Derazantinib plus gemcitabine in PDAC patients. Biomarker-driven patient stratification, for example based on FGFR expression or MUC5AC levels, may optimize response rates and facilitate precision medicine approaches. Additionally, further exploration into resistance mechanisms against FGFR inhibitors themselves remains warranted.
This seminal contribution by Ye, W. et al. represents a pivotal moment in the endeavor to subvert pancreatic cancer’s formidable defense mechanisms. By illuminating the molecular choreography by which Derazantinib dismantles pro-survival signaling and mucin-mediated protection, their work opens unprecedented avenues to amplify the impact of existing chemotherapy and improve the bleak prognosis associated with this disease.
In sum, this research charts a compelling course towards more effective treatment paradigms in PDAC, marshalling the power of molecular targeted therapies to reshape the future of pancreatic cancer care. With continued scientific momentum, the hope is that these insights will not only extend survival but also enhance the quality of life for countless patients battling this devastating malignancy.
Subject of Research: Enhancement of gemcitabine efficacy in pancreatic ductal adenocarcinoma (PDAC) through modulation of NF-κB and MAPK pathways to reduce MUC5AC expression.
Article Title: Derazantinib enhances gemcitabine efficacy in PDAC by attenuating the NF-κB and MAPK pathways to suppress MUC5AC expression.
Article References:
Ye, W., Huang, Y., Hong, L. et al. Derazantinib enhances gemcitabine efficacy in PDAC by attenuating the NF-κB and MAPK pathways to suppress MUC5AC expression. Med Oncol 43, 107 (2026). https://doi.org/10.1007/s12032-025-03222-1
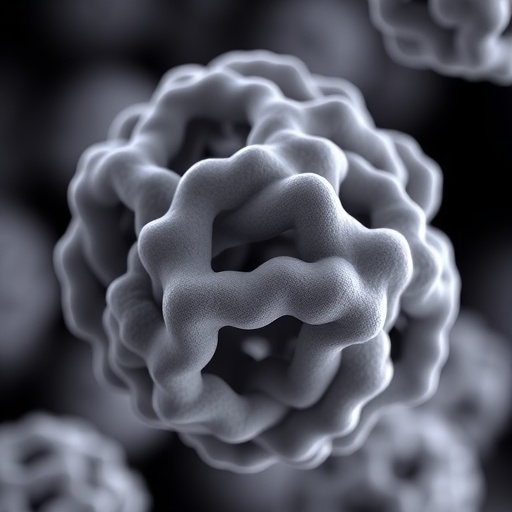
Image Credits: AI Generated
DOI: https://doi.org/10.1007/s12032-025-03222-1
Tags: cancer cell survival mechanismsDerazantinib and gemcitabine combination therapyenhancing chemotherapy efficacyfibroblast growth factor receptor inhibitionimproving survival rates in pancreatic cancermolecular targets in PDACMUC5AC protein suppression in cancerNF-κB and MAPK signaling pathwaysnovel therapeutic strategies for pancreatic canceroncological research advancementsovercoming drug resistance in pancreatic cancerpancreatic ductal adenocarcinoma treatment