In a groundbreaking study poised to reshape the therapeutic landscape of oncology, researchers have uncovered how ultrasound-stimulated microbubble cavitation can significantly enhance tumor perfusion and foster the normalization of tumor vasculature. This pioneering work, conducted on a rabbit VX2 tumor model, reveals a compelling mechanism by which focused ultrasound can modulate the tumor microenvironment to potentially improve the efficacy of cancer treatments.
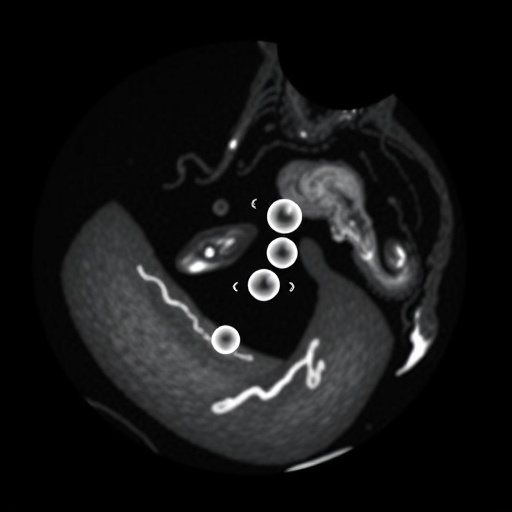
Tumors are notorious for their aberrant vascular structures — chaotic, leaky, and dysfunctional blood vessels that hinder effective drug delivery and oxygenation. This hostile microenvironment not only limits the success of chemotherapeutic and immunotherapeutic regimens but also fuels tumor progression and resistance. Addressing these issues, the study explores the innovative use of microbubbles, minuscule gas-filled spheres, in conjunction with ultrasound waves, to induce cavitation — the rapid oscillation and collapse of microbubbles — thereby mechanically influencing the tumor vasculature.
The researchers employed a rabbit VX2 tumor model, a well-established preclinical system that closely mimics the aggressive and vascular characteristics of human cancers. By carefully calibrating ultrasound parameters to stimulate microbubble cavitation without causing significant tissue damage, they observed a marked improvement in tumor blood flow. Enhanced perfusion was noted immediately after treatment and persisted for a duration that has critical implications for therapeutic windows.
At the core of this advancement lies the concept of vascular normalization — a therapeutic strategy aimed at restoring the structure and function of tumor blood vessels toward a more organized and efficient state. The study demonstrates that ultrasound-stimulated cavitation promotes this normalization process, reversing the chaotic architecture characteristic of malignant vasculature. Improved vessel integrity leads to better delivery of oxygen and nutrients, thereby alleviating hypoxic conditions that often drive tumor aggressiveness and therapy resistance.
Detailed histological analyses revealed that post-treatment tumors exhibited significantly reduced vessel permeability and increased pericyte coverage, indicative of stabilized and mature blood vessels. This contrasts sharply with the pre-treatment state where vessels showed fragility and leakiness. Such stabilization is crucial not only for drug delivery but also for minimizing interstitial pressure within tumors, which often impedes therapeutic agent penetration.
The mechanistic insights provided by the study suggest that the mechanical forces exerted by cavitating microbubbles stimulate endothelial cells lining the blood vessels, triggering signaling pathways conducive to vessel remodeling and repair. This biomechanical interaction paves the way for non-invasive modulation of tumor biology, harnessing physical forces to invoke biological responses favorable to treatment.
Clinically, these findings hold promise for synergistic cancer therapy approaches. Combining ultrasound-stimulated microbubble cavitation with chemotherapy, radiotherapy, or immunotherapy could overcome barriers posed by the dysfunctional tumor vasculature. Enhanced perfusion not only facilitates drug access but may also improve immune cell infiltration, amplifying anti-tumor immunity.
Importantly, the safety profile of this approach appears favorable. The study meticulously optimized ultrasound parameters to avoid tissue damage, with no significant adverse effects observed in normal surrounding tissues. This non-destructive modulation contrasts with traditional therapeutic methods that often carry high toxicity and collateral damage risks.
Furthermore, the ultrasound and microbubble strategy offers a highly controllable and targeted modality. Ultrasound can be precisely focused on tumor regions, allowing spatial and temporal control over treatment effects. Microbubbles, inherently confined to the vasculature, act as localized agents, minimizing systemic exposure and side effects.
The implications extend beyond oncology. The principles demonstrated here could be translated to other pathological conditions characterized by abnormal vasculature, such as cardiovascular diseases and wound healing disorders. Modulating blood vessel function non-invasively through ultrasound-mediated cavitation could become a versatile tool in regenerative medicine.
The study also raises intriguing questions about the interplay between mechanical forces and cellular signaling in the tumor microenvironment. Future research may unravel new molecular targets activated by cavitation-induced stresses, opening avenues for combination therapies that exploit these newly uncovered pathways.
In summary, this trailblazing investigation charts a promising course for augmenting cancer treatment through physical modulation of tumor blood vessels. Ultrasound-stimulated microbubble cavitation emerges as a powerful, non-invasive technique to improve tumor perfusion, promote vascular normalization, and ultimately enhance the delivery and efficacy of anti-cancer therapies.
As the oncology field increasingly embraces innovative strategies that transcend conventional pharmacology, the integration of biomechanical approaches such as this could redefine therapeutic paradigms. Clinical translation will require meticulous validation, but the foundational evidence presented provides robust optimism for the future of cancer care.
This research, heralding a fusion of physics, biology, and medicine, exemplifies the cutting edge of translational science. It underscores the potential of harnessing ultrasonics and microbubbles not just as diagnostic tools but as dynamic instruments of therapeutic transformation.
With further refinement and validation, ultrasound-stimulated microbubble cavitation might soon become a standard adjunct in oncological protocols, enhancing patient outcomes in ways previously unattainable. The convergence of technology and biology continues to unlock new frontiers that hold promise for conquering some of the most formidable challenges in medicine.
Subject of Research: Ultrasound-stimulated microbubble cavitation and its effects on tumor perfusion and vascular normalization in cancer therapy.
Article Title: Ultrasound-Stimulated microbubble cavitation improved tumor perfusion and promoted tumor vascular normalization in a rabbit VX2 tumor model.
Article References:
Luo, T., Bai, L., Yao, L. et al. Ultrasound-Stimulated microbubble cavitation improved tumor perfusion and promoted tumor vascular normalization in a rabbit VX2 tumor model. Med Oncol 43, 89 (2026). https://doi.org/10.1007/s12032-025-03226-x
Image Credits: AI Generated
DOI: https://doi.org/10.1007/s12032-025-03226-x
Tags: aberrant vascular structures in tumorschemotherapeutic regimens and resistanceimproving cancer treatment efficacyinnovative cancer research methodsmicrobubble cavitation mechanismpreclinical oncology studiesrabbit VX2 tumor modeltumor blood flow enhancementtumor vasculature normalizationultrasound microbubbles in cancer therapyultrasound parameters for tumor treatmentultrasound-stimulated drug delivery